Monday Poster Session
Category: Biliary/Pancreas
P1530 - A Comparison of Pancreatic Cyst Biopsy Techniques in a Patient With Serous Cystadenoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Matt Leupold, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Matt Leupold, MD1, Wei Chen, MD, PhD2, Somashekar Krishna, MD3
1The Ohio State University Wexner Medical Center, Columbus, OH; 2Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State Wexner Medical Center, Columbus, OH
Introduction: The prevalence of incidental pancreatic cystic lesions (PCLs) has been rising given an aging population and increased frequency of abdominal imaging. Due to this, various risk stratifying criteria have been developed to guide the management of these lesions and monitor for progression to pancreatic ductal adenocarcinoma. These guidelines often rely on endoscopic ultrasound (EUS) and fine needle aspiration (FNA) or biopsy (FNB) to further characterize high-risk PCLs. However, tissue yield is not always adequate and there is risk of non-diagnostic results. Advanced EUS diagnostics have included needle based confocal laser endomicroscopy (nCLE) and cyst fluid next generation sequencing analysis (NGS).
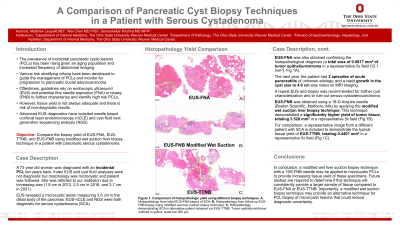
Case Description/Methods: A 73 year old woman was diagnosed with an incidental PCL ten years back. Index EUS and cyst fluid analyses were not diagnostic but morphology was microcystic and patient was followed. She was referred to our institution due to increasing size (1.8 cm in 2012, 2.5 cm in 2016, and 3.7 cm in 2021). EUS revealed microcystic lesion measuring 3.5 cm in the distal body of the pancreas. EUS-nCLE and NGS were both diagnostic for serous cystadenoma (SCA). EUS-FNA was also obtained confirming the histopathological diagnosis (a total area of 0.0817 mm2 of tumor epithelium/stroma in a representative 5x field [12.1 mm2], Fig A). The next year, patient had 2 episodes of acute pancreatitis of unknown etiology, and rapid growth in the cyst size to 4.6 cm by MRI imaging. A repeat EUS and biopsy was recommended to rule out malignant transformation. EUS-FNB was obtained using a 19-G Acquire needle (Boston Scientific, Marlboro, MA) by applying the modified wet suction liver biopsy technique. This technique demonstrated a significantly higher yield of tumor tissue, totaling 3.528 mm2 in a representative 5x field (Fig B). For comparison a representative image from a different patient with SCA is included to demonstrate the typical tissue yield of EUS-through-the-needle biopsy (TTNB), totaling 0.4407 mm2 in a representative 5x field (Fig C).
Discussion: In conclusion, a modified wet liver suction biopsy technique with a 19G FNB needle may be applied to microcystic PCLs to provide greater tissue yield. Future studies are required to determine if this technique will consistently provide a larger sample compared to EUS-FNA or EUS-TTNB. Importantly, a modified wet suction biopsy technique may provide an alternative technique for PCL biopsy of microcystic lesions that could reduce diagnostic uncertainty.

Disclosures:
Matt Leupold, MD1, Wei Chen, MD, PhD2, Somashekar Krishna, MD3. P1530 - A Comparison of Pancreatic Cyst Biopsy Techniques in a Patient With Serous Cystadenoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2Ohio State University Wexner Medical Center, Columbus, OH; 3The Ohio State Wexner Medical Center, Columbus, OH
Introduction: The prevalence of incidental pancreatic cystic lesions (PCLs) has been rising given an aging population and increased frequency of abdominal imaging. Due to this, various risk stratifying criteria have been developed to guide the management of these lesions and monitor for progression to pancreatic ductal adenocarcinoma. These guidelines often rely on endoscopic ultrasound (EUS) and fine needle aspiration (FNA) or biopsy (FNB) to further characterize high-risk PCLs. However, tissue yield is not always adequate and there is risk of non-diagnostic results. Advanced EUS diagnostics have included needle based confocal laser endomicroscopy (nCLE) and cyst fluid next generation sequencing analysis (NGS).
Case Description/Methods: A 73 year old woman was diagnosed with an incidental PCL ten years back. Index EUS and cyst fluid analyses were not diagnostic but morphology was microcystic and patient was followed. She was referred to our institution due to increasing size (1.8 cm in 2012, 2.5 cm in 2016, and 3.7 cm in 2021). EUS revealed microcystic lesion measuring 3.5 cm in the distal body of the pancreas. EUS-nCLE and NGS were both diagnostic for serous cystadenoma (SCA). EUS-FNA was also obtained confirming the histopathological diagnosis (a total area of 0.0817 mm2 of tumor epithelium/stroma in a representative 5x field [12.1 mm2], Fig A). The next year, patient had 2 episodes of acute pancreatitis of unknown etiology, and rapid growth in the cyst size to 4.6 cm by MRI imaging. A repeat EUS and biopsy was recommended to rule out malignant transformation. EUS-FNB was obtained using a 19-G Acquire needle (Boston Scientific, Marlboro, MA) by applying the modified wet suction liver biopsy technique. This technique demonstrated a significantly higher yield of tumor tissue, totaling 3.528 mm2 in a representative 5x field (Fig B). For comparison a representative image from a different patient with SCA is included to demonstrate the typical tissue yield of EUS-through-the-needle biopsy (TTNB), totaling 0.4407 mm2 in a representative 5x field (Fig C).
Discussion: In conclusion, a modified wet liver suction biopsy technique with a 19G FNB needle may be applied to microcystic PCLs to provide greater tissue yield. Future studies are required to determine if this technique will consistently provide a larger sample compared to EUS-FNA or EUS-TTNB. Importantly, a modified wet suction biopsy technique may provide an alternative technique for PCL biopsy of microcystic lesions that could reduce diagnostic uncertainty.

Figure: Figure A, Histopathology from initial EUS-FNA biopsy of SCA, tumor epithelium/stroma outlined in yellow, scale bar 200 µm
Figure B, Histopathology from follow-up EUS-FNB biopsy using modified wet liver suction biopsy technique, tumor epithelium/stroma outlined in yellow, scale bar 200 µm
Figure C, Histopathology demonstrating SCA in alternative patient obtained via EUS-TTNB, tumor epithelium/stroma outlined in yellow, scale bar 200 µm
Figure B, Histopathology from follow-up EUS-FNB biopsy using modified wet liver suction biopsy technique, tumor epithelium/stroma outlined in yellow, scale bar 200 µm
Figure C, Histopathology demonstrating SCA in alternative patient obtained via EUS-TTNB, tumor epithelium/stroma outlined in yellow, scale bar 200 µm
Disclosures:
Matt Leupold indicated no relevant financial relationships.
Wei Chen indicated no relevant financial relationships.
Somashekar Krishna: Mauna Kea Technologies – Grant/Research Support. Taewoong Medical USA – Grant/Research Support. US Biotest – Grant/Research Support.
Matt Leupold, MD1, Wei Chen, MD, PhD2, Somashekar Krishna, MD3. P1530 - A Comparison of Pancreatic Cyst Biopsy Techniques in a Patient With Serous Cystadenoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
