Monday Poster Session
Category: Biliary/Pancreas
P1532 - A Rare Case of Hemorrhagic Groove Pancreatitis Presenting as Duodenal Obstruction
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Tooba Laeeq, MD
University of Nevada, Las Vegas
Henderson, NV
Presenting Author(s)
Tooba Laeeq, MD1, Rajan Amin, MD2, Zahra Dossaji, DO3
1University of Nevada, Las Vegas, Henderson, NV; 2University of Nevada, Las Vegas, Las Vegas, NV; 3Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV
Introduction: Groove pancreatitis is an uncommon form of chronic pancreatitis affecting the groove between the duodenum, common bile duct and duodenum. Typically affecting men ages 40 to 50 with a history of smoking or alcohol use, it remains an uncommon finding.
Case Description/Methods: A 53-year-old male with past medical history of tobacco use presented with intractable nausea, vomiting and lower abdominal pain for 1 day. Physical exam revealed lower abdominal tenderness. Laboratory data included WBC 13 k/mm3, HGB 17 g/dl, Lipase 88 U/L, T Bili 0.5 mg/dl, AST 17 IU/L, ALT 19 U/L, Alk phos 104 U/L, A1c 11.3%. CT abdomen showed extensive pancreatic calcification with a 7 cm cystic lesion in the head of the pancreas/pancreaticoduodenal groove causing mass effect on the duodenum. EUS revealed atrophic pancreatic parenchyma and severe diffuse calcifications with dilation of the pancreatic duct and common bile duct. A large cystic lesion was noted within the duodenal wall causing mild obstruction of the duodenal lumen. FNA was attempted, but given the presence of bloody output the cyst was not fully drained. Repeat CT with oral contrast two days later re-demonstrated large cystic mass in the 2nd and 3rd part of the duodenum with nonspecific fat infiltration of the pancreatic duodenal groove. Patient was subsequently taken for repeat EUS for distal duodenal stent placement with relief of obstruction.
Discussion: Alcohol and smoking are known to increase the viscosity of pancreatic fluids, causing calcification in the pancreatic duct and impeding the flow of pancreatic fluids. This ultimately leads to fibrosis in the groove area, giving rise to groove pancreatitis. Its resemblance to pancreatic cancer on imaging poses a significant diagnostic challenge. Classic features on imaging include cystic transformation of the duodenum, paraduodenal cyst, duodenal wall thickening, and biliary ductal dilatation. Here we describe a case of groove pancreatitis causing mild duodenal obstruction, with relief of symptoms after duodenal stent placement. Treatment is typically conservative, but if symptoms are severe or persistent, interventional procedures such as stenting or pancreaticoduodenectomy can be attempted.

Disclosures:
Tooba Laeeq, MD1, Rajan Amin, MD2, Zahra Dossaji, DO3. P1532 - A Rare Case of Hemorrhagic Groove Pancreatitis Presenting as Duodenal Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Nevada, Las Vegas, Henderson, NV; 2University of Nevada, Las Vegas, Las Vegas, NV; 3Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV
Introduction: Groove pancreatitis is an uncommon form of chronic pancreatitis affecting the groove between the duodenum, common bile duct and duodenum. Typically affecting men ages 40 to 50 with a history of smoking or alcohol use, it remains an uncommon finding.
Case Description/Methods: A 53-year-old male with past medical history of tobacco use presented with intractable nausea, vomiting and lower abdominal pain for 1 day. Physical exam revealed lower abdominal tenderness. Laboratory data included WBC 13 k/mm3, HGB 17 g/dl, Lipase 88 U/L, T Bili 0.5 mg/dl, AST 17 IU/L, ALT 19 U/L, Alk phos 104 U/L, A1c 11.3%. CT abdomen showed extensive pancreatic calcification with a 7 cm cystic lesion in the head of the pancreas/pancreaticoduodenal groove causing mass effect on the duodenum. EUS revealed atrophic pancreatic parenchyma and severe diffuse calcifications with dilation of the pancreatic duct and common bile duct. A large cystic lesion was noted within the duodenal wall causing mild obstruction of the duodenal lumen. FNA was attempted, but given the presence of bloody output the cyst was not fully drained. Repeat CT with oral contrast two days later re-demonstrated large cystic mass in the 2nd and 3rd part of the duodenum with nonspecific fat infiltration of the pancreatic duodenal groove. Patient was subsequently taken for repeat EUS for distal duodenal stent placement with relief of obstruction.
Discussion: Alcohol and smoking are known to increase the viscosity of pancreatic fluids, causing calcification in the pancreatic duct and impeding the flow of pancreatic fluids. This ultimately leads to fibrosis in the groove area, giving rise to groove pancreatitis. Its resemblance to pancreatic cancer on imaging poses a significant diagnostic challenge. Classic features on imaging include cystic transformation of the duodenum, paraduodenal cyst, duodenal wall thickening, and biliary ductal dilatation. Here we describe a case of groove pancreatitis causing mild duodenal obstruction, with relief of symptoms after duodenal stent placement. Treatment is typically conservative, but if symptoms are severe or persistent, interventional procedures such as stenting or pancreaticoduodenectomy can be attempted.

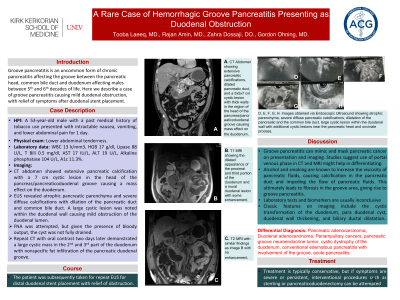
Figure: A. CT Abdomen showing extensive pancreatic calcifications, dilated pancreatic duct, and a 5x5x7 cm cystic lesion with thick walls in the region of the head of the pancreas/pancreaticoduodenal groove causing mass effect on the duodenum.
B. T1 MRI showing dilated appearance of proximal and third portion of duodenum and a mural duodenal lesion with some enhancement.
C. T2 MRI with similar findings as image B with no enhancement.
D, E, F, G, H. Images obtained via Endoscopic Ultrasound showing atrophic parenchyma, severe diffuse pancreatic calcifications, dilatation of the pancreatic and the common bile duct, large cystic lesion within the duodenal wall with additional cystic lesions near the pancreatic head and uncinate process.
B. T1 MRI showing dilated appearance of proximal and third portion of duodenum and a mural duodenal lesion with some enhancement.
C. T2 MRI with similar findings as image B with no enhancement.
D, E, F, G, H. Images obtained via Endoscopic Ultrasound showing atrophic parenchyma, severe diffuse pancreatic calcifications, dilatation of the pancreatic and the common bile duct, large cystic lesion within the duodenal wall with additional cystic lesions near the pancreatic head and uncinate process.
Disclosures:
Tooba Laeeq indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Zahra Dossaji indicated no relevant financial relationships.
Tooba Laeeq, MD1, Rajan Amin, MD2, Zahra Dossaji, DO3. P1532 - A Rare Case of Hemorrhagic Groove Pancreatitis Presenting as Duodenal Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
