Monday Poster Session
Category: Biliary/Pancreas
P1546 - Behind the Mask of Obstructive Jaundice: A Case of Lemmel’s Syndrome
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
.jpeg.jpg)
Mohammad A. Ahmed-Khan, MD
Danbury Hospital - Yale School of Medicine
Danbury, CT
Presenting Author(s)
Mohammad A. Ahmed-Khan, MD1, Chun Yu Peng, MD2, Joshua Freilich, 3, Zakee Jiffry, MD2, Mahnoor Hanif, MD4
1Danbury Hospital - Yale School of Medicine, Danbury, CT; 2Danbury Hospital, Danbury, CT; 3AUC School of Medicine, Danbury, CT; 4CMH Lahore Medical College, Lahore, Punjab, Pakistan
Introduction: Periampullary Diverticula (PAD) are anomalies of the small bowel in up to 27% of the population. Lemmel's Syndrome is defined as obstructive jaundice caused by a PAD compressing the intrapancreatic CBD with resultant bile duct dilatation for Lemmel's findings in 1934. 5-10% of these patients are symptomatic; although it is rare it needs to be on every clinician's differential. Commonly discovered incidental PAD are relatively benign, however once they become symptomatic the patients can have life-threatening presentations such as septic shock or obstructive jaundice without definitive cause leading to this being misdiagnosed.
Case Description/Methods: An 81-year-old Vietnamese female without significant past medical or surgical history presented to the ED for abdominal pain, nausea, vomiting and fevers for 1 day. She was febrile and tachycardic in the ED and on physical examination she had significant right upper quadrant pain without guarding or distention. LFTs showed an elevated Total Bilirubin of 2.1, Direct 1.0, AST 277, ALT 132, abdominal ultrasound: CBD dilation to 12 mm. MRCP confirmed CBD dilation and showed large PAD, confirmation CT scan showed dilated common bile duct 12 mm with moderate intrahepatic biliary duct dilation, large PAD without obstructing choledocholithiasis. She was admitted for severe sepsis treated with antibiotics and fluids; the patient rapidly improved and therefore ERCP was no longer necessary. The patient was scheduled for follow-up with HPB surgery and GI and subsequently discharged.
Discussion: Only a fraction of patients with PAD become symptomatic thus creating a diagnostic dilemma is PAD can cause biliary obstruction by sphincter dysfunction, direct or extrinsic compression (by fluid or debris). This is why a strong differential diagnosis, radiologic imaging (CT/MRI/MRCP), or direct visualization with endoscopy can aid clinicians to diagnose this rare syndrome. Currently diagnostic and therapeutic endoscopy with a side-viewing duodenoscope is the superior option and ERCP is heralded as the gold standard of treatment based on Li-Tanaka classification. The treatment of this condition is categorized into mild and severe symptoms, mild cases use diet modification or even diverticular lavage offering complete resolution of symptoms however in more severe cases endoscopic biliary cannulation and sphincterotomy provide adequate relief and circumvent the need for invasive surgical intervention as previously surgery was the only option.

Disclosures:
Mohammad A. Ahmed-Khan, MD1, Chun Yu Peng, MD2, Joshua Freilich, 3, Zakee Jiffry, MD2, Mahnoor Hanif, MD4. P1546 - Behind the Mask of Obstructive Jaundice: A Case of Lemmel’s Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Danbury Hospital - Yale School of Medicine, Danbury, CT; 2Danbury Hospital, Danbury, CT; 3AUC School of Medicine, Danbury, CT; 4CMH Lahore Medical College, Lahore, Punjab, Pakistan
Introduction: Periampullary Diverticula (PAD) are anomalies of the small bowel in up to 27% of the population. Lemmel's Syndrome is defined as obstructive jaundice caused by a PAD compressing the intrapancreatic CBD with resultant bile duct dilatation for Lemmel's findings in 1934. 5-10% of these patients are symptomatic; although it is rare it needs to be on every clinician's differential. Commonly discovered incidental PAD are relatively benign, however once they become symptomatic the patients can have life-threatening presentations such as septic shock or obstructive jaundice without definitive cause leading to this being misdiagnosed.
Case Description/Methods: An 81-year-old Vietnamese female without significant past medical or surgical history presented to the ED for abdominal pain, nausea, vomiting and fevers for 1 day. She was febrile and tachycardic in the ED and on physical examination she had significant right upper quadrant pain without guarding or distention. LFTs showed an elevated Total Bilirubin of 2.1, Direct 1.0, AST 277, ALT 132, abdominal ultrasound: CBD dilation to 12 mm. MRCP confirmed CBD dilation and showed large PAD, confirmation CT scan showed dilated common bile duct 12 mm with moderate intrahepatic biliary duct dilation, large PAD without obstructing choledocholithiasis. She was admitted for severe sepsis treated with antibiotics and fluids; the patient rapidly improved and therefore ERCP was no longer necessary. The patient was scheduled for follow-up with HPB surgery and GI and subsequently discharged.
Discussion: Only a fraction of patients with PAD become symptomatic thus creating a diagnostic dilemma is PAD can cause biliary obstruction by sphincter dysfunction, direct or extrinsic compression (by fluid or debris). This is why a strong differential diagnosis, radiologic imaging (CT/MRI/MRCP), or direct visualization with endoscopy can aid clinicians to diagnose this rare syndrome. Currently diagnostic and therapeutic endoscopy with a side-viewing duodenoscope is the superior option and ERCP is heralded as the gold standard of treatment based on Li-Tanaka classification. The treatment of this condition is categorized into mild and severe symptoms, mild cases use diet modification or even diverticular lavage offering complete resolution of symptoms however in more severe cases endoscopic biliary cannulation and sphincterotomy provide adequate relief and circumvent the need for invasive surgical intervention as previously surgery was the only option.

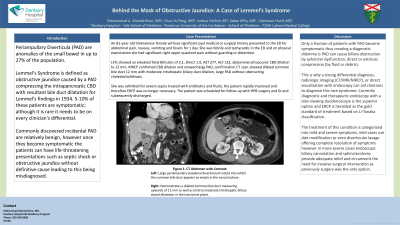
Figure: CT scan Abdomen with Contrast:
Left: Large periampullary duodenal diverticulum noted into which the common bile duct appears to empty in the coronal plane.
Right: Demonstrates a dilated common bile duct measuring upwards of 11 mm as well as mild to moderate intrahepatic biliary ductal dilatation in the transverse plane.
Left: Large periampullary duodenal diverticulum noted into which the common bile duct appears to empty in the coronal plane.
Right: Demonstrates a dilated common bile duct measuring upwards of 11 mm as well as mild to moderate intrahepatic biliary ductal dilatation in the transverse plane.
Disclosures:
Mohammad Ahmed-Khan indicated no relevant financial relationships.
Chun Yu Peng indicated no relevant financial relationships.
Joshua Freilich indicated no relevant financial relationships.
Zakee Jiffry indicated no relevant financial relationships.
Mahnoor Hanif indicated no relevant financial relationships.
Mohammad A. Ahmed-Khan, MD1, Chun Yu Peng, MD2, Joshua Freilich, 3, Zakee Jiffry, MD2, Mahnoor Hanif, MD4. P1546 - Behind the Mask of Obstructive Jaundice: A Case of Lemmel’s Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
