Monday Poster Session
Category: Biliary/Pancreas
P1552 - A Rare Case of Metastatic Primary Gallbladder Squamous Cell Carcinoma in a Patient With Primary Sclerosing Cholangitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- RS
Rachel Schwartz, DO
Texas Institute for Graduate Medical Education and Research
San Antonio, TX
Presenting Author(s)
Rachel Schwartz, DO1, Matthew Schwartz, MD2, Alexander Wilson, MD2, Anish Patel, DO2, Geoff Bader, MD2
1Texas Institute for Graduate Medical Education and Research, San Antonio, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Primary sclerosing cholangitis (PSC) is a major risk factor for malignancy, especially in the setting of ulcerative colitis (UC). While most biliary malignancies are adenocarcinomas, squamous cell carcinoma (SCC) can rarely occur. We present a rare case of primary gallbladder (GB) SCC with hepatic metastases in a patient with PSC and UC.
Case Description/Methods: A 55-year-old female with history of PSC and UC was evaluated for 5 days of non-specific abdominal pain. Her surgical history included a total proctocolectomy for pancolitis with low-grade dysplasia complicated by recurrent pouchitis treated with ustekinumab. She was afebrile with labs notable for a normal white blood cell count and mild, stable elevations in alkaline phosphatase and bilirubin. Computed tomography (CT) revealed two peripherally enhancing, hypo-attenuated hepatic lesions with septation favored to represent abscesses, along with a suspected vascular irregularity along the medial GB wall. Interventional radiology guided aspiration of the liver lesions revealed atypical cells and keratinization concerning for SCC, subsequently confirmed on repeat core biopsy. Evaluation for a primary source was non-diagnostic, including anoscopy, upper endoscopy, laryngoscopy, chest CT, transvaginal ultrasound, pap smear, and endometrial biopsy. A positron emission tomography and CT scan revealed increased uptake at the GB. Endoscopic ultrasound showed eccentric GB thickening, with biopsy confirming a primary GB SCC. Our patient opted to pursue palliative chemotherapy.
Discussion: SCC in the liver should always raise concern for metastasis, as primary SCC of the liver is exceedingly rare. While cholangiocarcinoma infrequently presents as SCC or adenosquamous, pure GB SCC accounts for only 3% of all GB cancers and carries a poor prognosis. PSC patients with or without inflammatory bowel disease (IBD) have an increased risk of biliary malignancy and should be screened annually with abdominal imaging, ideally magnetic resonance imaging with cholangiopancreatography. Our patient had recently experienced an unrelated medical issue that had delayed her screening by a few months. Radiologic features of GB cancer can be highly variable, with a minority demonstrating focal, asymmetric wall thickening with contrast enhancement. While our case is of a rare variant of GB cancer, it highlights the importance of screening for biliary cancer in the PSC-IBD population.

Disclosures:
Rachel Schwartz, DO1, Matthew Schwartz, MD2, Alexander Wilson, MD2, Anish Patel, DO2, Geoff Bader, MD2. P1552 - A Rare Case of Metastatic Primary Gallbladder Squamous Cell Carcinoma in a Patient With Primary Sclerosing Cholangitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Institute for Graduate Medical Education and Research, San Antonio, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Primary sclerosing cholangitis (PSC) is a major risk factor for malignancy, especially in the setting of ulcerative colitis (UC). While most biliary malignancies are adenocarcinomas, squamous cell carcinoma (SCC) can rarely occur. We present a rare case of primary gallbladder (GB) SCC with hepatic metastases in a patient with PSC and UC.
Case Description/Methods: A 55-year-old female with history of PSC and UC was evaluated for 5 days of non-specific abdominal pain. Her surgical history included a total proctocolectomy for pancolitis with low-grade dysplasia complicated by recurrent pouchitis treated with ustekinumab. She was afebrile with labs notable for a normal white blood cell count and mild, stable elevations in alkaline phosphatase and bilirubin. Computed tomography (CT) revealed two peripherally enhancing, hypo-attenuated hepatic lesions with septation favored to represent abscesses, along with a suspected vascular irregularity along the medial GB wall. Interventional radiology guided aspiration of the liver lesions revealed atypical cells and keratinization concerning for SCC, subsequently confirmed on repeat core biopsy. Evaluation for a primary source was non-diagnostic, including anoscopy, upper endoscopy, laryngoscopy, chest CT, transvaginal ultrasound, pap smear, and endometrial biopsy. A positron emission tomography and CT scan revealed increased uptake at the GB. Endoscopic ultrasound showed eccentric GB thickening, with biopsy confirming a primary GB SCC. Our patient opted to pursue palliative chemotherapy.
Discussion: SCC in the liver should always raise concern for metastasis, as primary SCC of the liver is exceedingly rare. While cholangiocarcinoma infrequently presents as SCC or adenosquamous, pure GB SCC accounts for only 3% of all GB cancers and carries a poor prognosis. PSC patients with or without inflammatory bowel disease (IBD) have an increased risk of biliary malignancy and should be screened annually with abdominal imaging, ideally magnetic resonance imaging with cholangiopancreatography. Our patient had recently experienced an unrelated medical issue that had delayed her screening by a few months. Radiologic features of GB cancer can be highly variable, with a minority demonstrating focal, asymmetric wall thickening with contrast enhancement. While our case is of a rare variant of GB cancer, it highlights the importance of screening for biliary cancer in the PSC-IBD population.

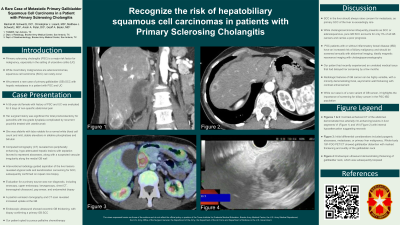
Figure: Fig. 1: Contrast-enhanced CT of the abdomen demonstrated two arterially rim-enhancing lesions in liver segments VI (A) and VIII (B) with internal hypoattenuation suggesting necrosis. Initial differential considerations included pyogenic abscesses, metastases, or primary liver malignancy. Whole-body 18F-FDG PET/CT showed gallbladder distention with marked thickening and avidity of the gallbladder neck (C, D). CT demonstrating heavily enhancing focus of gallbladder wall thickening, which initially raised concern for pseudoaneurysm or other vascular pathology (E). Endoscopic ultrasound demonstrating thickening of gallbladder neck, biopsied (F).
Disclosures:
Rachel Schwartz indicated no relevant financial relationships.
Matthew Schwartz indicated no relevant financial relationships.
Alexander Wilson indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Geoff Bader indicated no relevant financial relationships.
Rachel Schwartz, DO1, Matthew Schwartz, MD2, Alexander Wilson, MD2, Anish Patel, DO2, Geoff Bader, MD2. P1552 - A Rare Case of Metastatic Primary Gallbladder Squamous Cell Carcinoma in a Patient With Primary Sclerosing Cholangitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
