Monday Poster Session
Category: Biliary/Pancreas
P1567 - Fat or Foe: Unprovoked Hypertriglyceridemia-Induced Recurrent Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Tripti Nagar, MD
Wayne State University
Detroit, MI
Presenting Author(s)
Tripti Nagar, MD1, Issam Turk, MD2
1Wayne State University, Detroit, MI; 2Ascension Providence Rochester Hospital, Rochester, MI
Introduction: Hypertriglyceridemia (HTG) is seen in approximately 7% of acute pancreatitis patients, more commonly in those with existing dyslipidemia. Although diabetes is a known secondary predisposing factor, acute HTG without personal history changes is rare. We present the first case to our knowledge of recurrent acute pancreatitis due to acute type I HTG in a patient with otherwise normal serum triglycerides (TGs).
Case Description/Methods: Our patient is a 40-year-old female with type 2 diabetes mellitus and dyslipidemia on optimal therapy with fenofibrate and omega-3 acids. She was evaluated inpatient for acute epigastric abdominal pain, nausea and vomiting. Her low fat diet only included avocado oil intermittently. She denied new medications, alcohol, IV drug abuse, hepatitis, tattoo history, herbal supplements, NSAIDs, antibiotics, ill contacts, recent travel or new food intake. She did not have a family history of malignancy. Surgical history included cholecystectomy. Further laboratory evaluation diagnosed acute pancreatitis. She has had 10 recurrent episodes since 2012. During each acute flare, TG levels would spike past measurable levels. Autoimmune workup and fecal elastase were negative, along with evaluation for any other metabolic, viral or bacterial causes. Treatment with aggressive IV fluids and an insulin drip was recommended, however, adamantly refused the insulin drip for concerns of hypoglycemia. She also declined plasmapheresis. Her TG levels rapidly corrected with IV fluids, with resolution over the course of 3 days. CT scan after her acute flare showed no signs of chronic pancreatitis. She was discharged without complications.
Discussion: Despite thorough clinical evaluation and medical history review, our patient continued to have unprovoked spikes in TGs causing acute pancreatitis. Optimal therapy with fenofibrate and omega-3 acids kept her baseline lipid panel normal, significantly reducing her risk of pancreatitis. Dietary modifications were also strictly upheld with fat intake < 20 g/day. Traditional treatment with an insulin drip or plasmapheresis was not required. Fluid hydration was sufficient to normalize TG and lipase levels. This posed a unique clinical situation as preventative practices showed minimal benefit. Some studies suggest the use of routine plasmapheresis in patients with a baseline elevation in TG. However, there is minimal data demonstrating effective prevention of pancreatitis and acute TG elevations in a patient with an optimized diet and medical therapy.

Disclosures:
Tripti Nagar, MD1, Issam Turk, MD2. P1567 - Fat or Foe: Unprovoked Hypertriglyceridemia-Induced Recurrent Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University, Detroit, MI; 2Ascension Providence Rochester Hospital, Rochester, MI
Introduction: Hypertriglyceridemia (HTG) is seen in approximately 7% of acute pancreatitis patients, more commonly in those with existing dyslipidemia. Although diabetes is a known secondary predisposing factor, acute HTG without personal history changes is rare. We present the first case to our knowledge of recurrent acute pancreatitis due to acute type I HTG in a patient with otherwise normal serum triglycerides (TGs).
Case Description/Methods: Our patient is a 40-year-old female with type 2 diabetes mellitus and dyslipidemia on optimal therapy with fenofibrate and omega-3 acids. She was evaluated inpatient for acute epigastric abdominal pain, nausea and vomiting. Her low fat diet only included avocado oil intermittently. She denied new medications, alcohol, IV drug abuse, hepatitis, tattoo history, herbal supplements, NSAIDs, antibiotics, ill contacts, recent travel or new food intake. She did not have a family history of malignancy. Surgical history included cholecystectomy. Further laboratory evaluation diagnosed acute pancreatitis. She has had 10 recurrent episodes since 2012. During each acute flare, TG levels would spike past measurable levels. Autoimmune workup and fecal elastase were negative, along with evaluation for any other metabolic, viral or bacterial causes. Treatment with aggressive IV fluids and an insulin drip was recommended, however, adamantly refused the insulin drip for concerns of hypoglycemia. She also declined plasmapheresis. Her TG levels rapidly corrected with IV fluids, with resolution over the course of 3 days. CT scan after her acute flare showed no signs of chronic pancreatitis. She was discharged without complications.
Discussion: Despite thorough clinical evaluation and medical history review, our patient continued to have unprovoked spikes in TGs causing acute pancreatitis. Optimal therapy with fenofibrate and omega-3 acids kept her baseline lipid panel normal, significantly reducing her risk of pancreatitis. Dietary modifications were also strictly upheld with fat intake < 20 g/day. Traditional treatment with an insulin drip or plasmapheresis was not required. Fluid hydration was sufficient to normalize TG and lipase levels. This posed a unique clinical situation as preventative practices showed minimal benefit. Some studies suggest the use of routine plasmapheresis in patients with a baseline elevation in TG. However, there is minimal data demonstrating effective prevention of pancreatitis and acute TG elevations in a patient with an optimized diet and medical therapy.

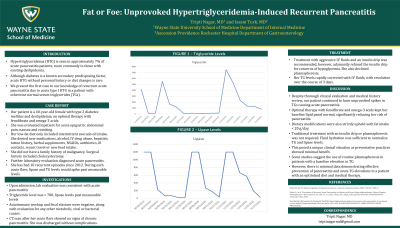
Figure: Lipase and triglyceride trends during inpatient admissions as well as established outpatient baseline labs.
Disclosures:
Tripti Nagar indicated no relevant financial relationships.
Issam Turk indicated no relevant financial relationships.
Tripti Nagar, MD1, Issam Turk, MD2. P1567 - Fat or Foe: Unprovoked Hypertriglyceridemia-Induced Recurrent Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
