Monday Poster Session
Category: Biliary/Pancreas
P1574 - EBV-Induced Hepatitis With Extrinsic Biliary Stricturing
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Timothy Graziano, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Timothy Graziano, DO1, William Ghaul, DO1, Chandler Patton, DO1, Amanda Jacubowsky, DO, MSMEd1, Janson Jacob, MD1, Travis Magdaleno, DO1, Shashin Shah, MD2
1Lehigh Valley Health Network, Allentown, PA; 2Eastern Pennsylvania Gastrointestinal and Liver Specialists, Allentown, PA
Introduction: Epstein-Barr virus (EBV)-associated hepatitis is a very common but typically subclinical and self-limited disease, especially in immunocompetent patients. Severe complications have been documented, but such cases are very infrequent. Here, we present a rare case of EBV in an immunocompetent patient causing significant cholestasis secondary to a biliary stricture.
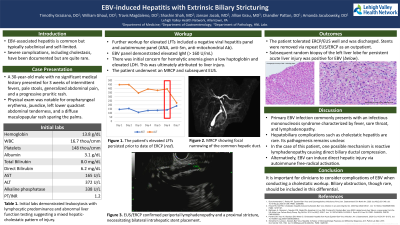
Case Description/Methods: A 30-year-old male with no significant past medical history presented with 3 weeks of intermittent fevers, jaundice, pale stools, abdominal pain, and a progressive pruritic rash. On presentation, the patient demonstrated jaundice with left lower quadrant abdominal tenderness and a diffuse maculopapular rash sparing the palms. Initial labs revealed leukocytosis with lymphocytic predominance (13.7 thou/cmm), elevated AST (165 U/L), ALT (372 U/L), alkaline phosphatase (338 U/L), total bilirubin (8.0 mg/dL) and direct bilirubin (6.2 mg/dL) levels, elevated lactate dehydrogenase (598 U/L), and decreased haptoglobin (< 3 mg/dL). A comprehensive autoimmune workup was negative. Serum EBV IgM was positive. GI was consulted, and MRCP revealed focal narrowing of the superior common hepatic duct. The patient underwent EUS/ERCP, which revealed significant periportal lymphadenopathy. Cholangiogram confirmed a proximal stricture and bilateral intrahepatic stents were placed. Following discharge, the patient underwent repeat EUS/ERCP for intrahepatic stent removal and liver biopsy for persistently elevated transaminases. Pathology was consistent with EBV-associated cholestatic hepatitis. The patient’s symptoms and lab abnormalities eventually resolved, and he continued to follow with Hepatology in the outpatient setting.
Discussion: Primary EBV infection classically presents with an infectious mononucleosis syndrome characterized by sore throat, fever, and lymphadenopathy, among other nonspecific findings. Cholestatic hepatitis is a very uncommon manifestation of this condition, and its exact pathogenesis remains unclear. In the case of our patient, one possible mechanism precipitating cholestasis may be reactive periportal lymphadenopathy causing direct biliary ductal compression. EBV is also known to induce direct hepatic injury via autoimmune-mediated free radical activation, suggesting an alternative or perhaps a concomitant explanation. Though exceptionally rare, it is important to consider these pathophysiological responses when conducting a cholestatic workup.
Disclosures:
Timothy Graziano, DO1, William Ghaul, DO1, Chandler Patton, DO1, Amanda Jacubowsky, DO, MSMEd1, Janson Jacob, MD1, Travis Magdaleno, DO1, Shashin Shah, MD2. P1574 - EBV-Induced Hepatitis With Extrinsic Biliary Stricturing, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lehigh Valley Health Network, Allentown, PA; 2Eastern Pennsylvania Gastrointestinal and Liver Specialists, Allentown, PA
Introduction: Epstein-Barr virus (EBV)-associated hepatitis is a very common but typically subclinical and self-limited disease, especially in immunocompetent patients. Severe complications have been documented, but such cases are very infrequent. Here, we present a rare case of EBV in an immunocompetent patient causing significant cholestasis secondary to a biliary stricture.
Case Description/Methods: A 30-year-old male with no significant past medical history presented with 3 weeks of intermittent fevers, jaundice, pale stools, abdominal pain, and a progressive pruritic rash. On presentation, the patient demonstrated jaundice with left lower quadrant abdominal tenderness and a diffuse maculopapular rash sparing the palms. Initial labs revealed leukocytosis with lymphocytic predominance (13.7 thou/cmm), elevated AST (165 U/L), ALT (372 U/L), alkaline phosphatase (338 U/L), total bilirubin (8.0 mg/dL) and direct bilirubin (6.2 mg/dL) levels, elevated lactate dehydrogenase (598 U/L), and decreased haptoglobin (< 3 mg/dL). A comprehensive autoimmune workup was negative. Serum EBV IgM was positive. GI was consulted, and MRCP revealed focal narrowing of the superior common hepatic duct. The patient underwent EUS/ERCP, which revealed significant periportal lymphadenopathy. Cholangiogram confirmed a proximal stricture and bilateral intrahepatic stents were placed. Following discharge, the patient underwent repeat EUS/ERCP for intrahepatic stent removal and liver biopsy for persistently elevated transaminases. Pathology was consistent with EBV-associated cholestatic hepatitis. The patient’s symptoms and lab abnormalities eventually resolved, and he continued to follow with Hepatology in the outpatient setting.
Discussion: Primary EBV infection classically presents with an infectious mononucleosis syndrome characterized by sore throat, fever, and lymphadenopathy, among other nonspecific findings. Cholestatic hepatitis is a very uncommon manifestation of this condition, and its exact pathogenesis remains unclear. In the case of our patient, one possible mechanism precipitating cholestasis may be reactive periportal lymphadenopathy causing direct biliary ductal compression. EBV is also known to induce direct hepatic injury via autoimmune-mediated free radical activation, suggesting an alternative or perhaps a concomitant explanation. Though exceptionally rare, it is important to consider these pathophysiological responses when conducting a cholestatic workup.
Disclosures:
Timothy Graziano indicated no relevant financial relationships.
William Ghaul indicated no relevant financial relationships.
Chandler Patton indicated no relevant financial relationships.
Amanda Jacubowsky indicated no relevant financial relationships.
Janson Jacob indicated no relevant financial relationships.
Travis Magdaleno indicated no relevant financial relationships.
Shashin Shah indicated no relevant financial relationships.
Timothy Graziano, DO1, William Ghaul, DO1, Chandler Patton, DO1, Amanda Jacubowsky, DO, MSMEd1, Janson Jacob, MD1, Travis Magdaleno, DO1, Shashin Shah, MD2. P1574 - EBV-Induced Hepatitis With Extrinsic Biliary Stricturing, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
