Monday Poster Session
Category: Biliary/Pancreas
P1575 - A Rare Presentation of Drug-Induced Pancreatitis After Cyclophosphamide Infusion
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- MO
Mark Obri, MD
Henry Ford Hospital
Detroit, Michigan
Presenting Author(s)
Mark Obri, MD1, Sanad Dawod, MD1, Austin Qasawa, BS2, Alan Fahoury, BS3, Johnathan Stephan, MD1, Wasih Kamran, MD1, Syed-Mohammed Jafri, MD4
1Henry Ford Hospital, Detroit, MI; 2Wayne State University, College of Medicine, Detroit, MI; 3University of Toledo, College of Medicine, Detroit, MI; 4Henry Ford Health System, Detroit, MI
Introduction: Acute pancreatitis makes up a significant amount of admissions and emergency room visits in the United States. Admissions vary in acuity and etiology. Drug induced pancreatitis make up a minority of cases, but are important to recognize as treatment involves withdrawing the offending agent. We present a rare case of cyclophosphamide induced pancreatitis in a patient who received their sixth dose with a history Systemic Lupus Erythematous (SLE).
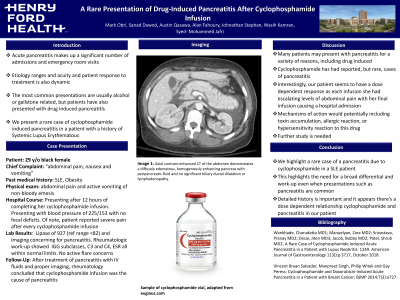
Case Description/Methods: A 29 year old female with past medical history of SLE, End-stage-renal Disease (ESRD) and hypertension who presented to the ED with significant nausea and vomiting. She stated that she had multiple episodes of nausea and vomiting 12 hours after completion of her cytotaxan infusion and elevated blood pressure. Patient presented with a BP of 225/153 with no focal deficits and complained of significant abdominal pain. Patient was found to have a lipase of 927 (IU/L ref range < 82) and imaging concerning for autoimmune pancreatitis. CT of the abdomen demonstrated a diffusely enlarged and edematous pancreas with peripancreatic fluid concerning for autoimmune pancreatitis but did not show any biliary duct or gallbladder abnormalities. Of note, patient did report numerous episodes of abdominal pain with her Cytotaxan effusion that she dismissed as cramps or gastric issues. She received a total of 6 doses with her last dose being prior to presentation. Patient’s physical exam and review of system were significant only for abdominal pain and nausea and vomiting.
Rheumatologic work-up showed normal IGG subclasses, C3 and C4 within normal limits and a normal Erythrocyte Sedimentation Rate. Abnormal labs included C-reactive protein 1.3mg/dl (refrence normal < 0.5mg/dl). Rheumatology and Neurology were consulted and agreed that the patient was not in an active flare of Lupus and with her immunologic/rheumatologic labs demonstrating normal values, believed this to be from her recent cyclophosphamide infusion. Interestingly, patient reported abdominal pain after every infusion of her cyclophosphamide.
Discussion: We present a rare presentation of pancreatitis due to cyclophosphamide. Drug induced pancreatitis should always be on the differential in the case of acute pancreatitis. Few cases have demonstrated this presentation due to cyclophosphamide. Interestingly, the patient tolerated the first 5 doses with only minor abdominal pain. This demonstrates the need to keep a broad differential and have extensive medication review.
Disclosures:
Mark Obri, MD1, Sanad Dawod, MD1, Austin Qasawa, BS2, Alan Fahoury, BS3, Johnathan Stephan, MD1, Wasih Kamran, MD1, Syed-Mohammed Jafri, MD4. P1575 - A Rare Presentation of Drug-Induced Pancreatitis After Cyclophosphamide Infusion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Wayne State University, College of Medicine, Detroit, MI; 3University of Toledo, College of Medicine, Detroit, MI; 4Henry Ford Health System, Detroit, MI
Introduction: Acute pancreatitis makes up a significant amount of admissions and emergency room visits in the United States. Admissions vary in acuity and etiology. Drug induced pancreatitis make up a minority of cases, but are important to recognize as treatment involves withdrawing the offending agent. We present a rare case of cyclophosphamide induced pancreatitis in a patient who received their sixth dose with a history Systemic Lupus Erythematous (SLE).
Case Description/Methods: A 29 year old female with past medical history of SLE, End-stage-renal Disease (ESRD) and hypertension who presented to the ED with significant nausea and vomiting. She stated that she had multiple episodes of nausea and vomiting 12 hours after completion of her cytotaxan infusion and elevated blood pressure. Patient presented with a BP of 225/153 with no focal deficits and complained of significant abdominal pain. Patient was found to have a lipase of 927 (IU/L ref range < 82) and imaging concerning for autoimmune pancreatitis. CT of the abdomen demonstrated a diffusely enlarged and edematous pancreas with peripancreatic fluid concerning for autoimmune pancreatitis but did not show any biliary duct or gallbladder abnormalities. Of note, patient did report numerous episodes of abdominal pain with her Cytotaxan effusion that she dismissed as cramps or gastric issues. She received a total of 6 doses with her last dose being prior to presentation. Patient’s physical exam and review of system were significant only for abdominal pain and nausea and vomiting.
Rheumatologic work-up showed normal IGG subclasses, C3 and C4 within normal limits and a normal Erythrocyte Sedimentation Rate. Abnormal labs included C-reactive protein 1.3mg/dl (refrence normal < 0.5mg/dl). Rheumatology and Neurology were consulted and agreed that the patient was not in an active flare of Lupus and with her immunologic/rheumatologic labs demonstrating normal values, believed this to be from her recent cyclophosphamide infusion. Interestingly, patient reported abdominal pain after every infusion of her cyclophosphamide.
Discussion: We present a rare presentation of pancreatitis due to cyclophosphamide. Drug induced pancreatitis should always be on the differential in the case of acute pancreatitis. Few cases have demonstrated this presentation due to cyclophosphamide. Interestingly, the patient tolerated the first 5 doses with only minor abdominal pain. This demonstrates the need to keep a broad differential and have extensive medication review.
Disclosures:
Mark Obri indicated no relevant financial relationships.
Sanad Dawod indicated no relevant financial relationships.
Austin Qasawa indicated no relevant financial relationships.
Alan Fahoury indicated no relevant financial relationships.
Johnathan Stephan indicated no relevant financial relationships.
Wasih Kamran indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie – Advisor or Review Panel Member, Speakers Bureau.
Mark Obri, MD1, Sanad Dawod, MD1, Austin Qasawa, BS2, Alan Fahoury, BS3, Johnathan Stephan, MD1, Wasih Kamran, MD1, Syed-Mohammed Jafri, MD4. P1575 - A Rare Presentation of Drug-Induced Pancreatitis After Cyclophosphamide Infusion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
