Monday Poster Session
Category: Colon
P1588 - Risk Factors for Fecal Microbiota Transplant Failure and Their Utility in Predicting FMT Outcomes: A Nationwide Retrospective Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Hisham Hussan, MD
University of California Davis
Sacramento, CA
Presenting Author(s)
Hisham Hussan, MD1, Saleh Al-Juburi, BS2, Sean K. Romeo, BS1, Mohamed Ali, MD1, Hazem Shamseddeen, MD1, Kelci Coe, MPH3, ChienWei Chiang, PhD4, Erica Reed, PharmD3
1University of California Davis, Sacramento, CA; 2Wayne State University School of Medicine, Folsom, CA; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4College of Medicine, The Ohio State University, Columbus, OH
Introduction: C. difficile is one of the most common causes of healthcare-associated infection, often complicated by recurrent or severe C. difficile infections (CDI). Fecal microbiota transplant (FMT) is a well-established and effective treatment for recalcitrant CDI. However, not all patients successfully resolve CDI after FMT – a challenging clinical outcome. As CDI rates continue to rise, we investigated risk factors and predictors of FMT failure.
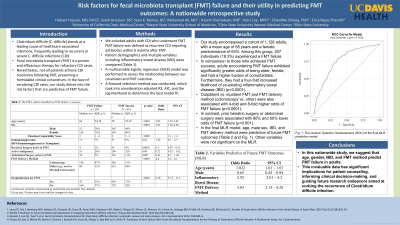
Methods: This retrospective cohort study used the 2012-2020 MarketScan database. Using billing codes, we included adults with CDI who underwent an FMT. FMT failure was defined as recurrent CDI requiring antibiotics within 6 months after FMT. Patient demographics and multiple variables including inflammatory bowel disease (IBD) were compared (Table 1). A multivariable logistic regression (MLR) model was performed to assess the relationship between our covariates and FMT outcome. We included variables in the MLR model if they were statistically significant at the univariate level. A forward selection method was conducted, which took into consideration adjusted R2, AIC, and the log-likelihood to determine the best model fit. Statistical significance was defined as a p< 0.05.
Results: Our FMT cohort included 1,126 adults (mean age of 58 years, 63% females), of which 207 (18.3%) had a failed FMT. Compared to FMT success, adults with FMT failure had higher odds of being older, females, with more comorbidities, and four-fold higher odds of co-existing IBD (P< 0.0001). Outpatient vs. inpatient FMT and FMT delivery method (colonoscopy vs. other) were also associated with 4-fold and 8-fold higher odds of FMT failure, respectively (p< 0.0001). In contrast, a history of bariatric surgery was associated with 80% lower odds of FMT failure (p< 0.001). Immunosuppression, body mass index categories, pregnancy, malignancy, and prior CDI number were not associated with our FMT outcomes. In the final MLR model, age [odds ratio (OR) 1.022; 95%CI,1.01-1.03], male sex (OR 0.65; 95% CI, 0.45-0.94), IBD (OR 2.92; 95% CI, 2.01-4.2), and FMT delivery method (OR 3.03; 95%CI, 2.15-4.28) were predictive of future FMT outcomes. Other variables were not significant on the MLR. Fig. 1 illustrates our MLR model's diagnostic ability.
Discussion: In this nationwide study, we suggest that age, sex, IBD, and FMT method can predict adults who will have an FMT failure. This data is critical for patient counseling, clinical decision-making, and future studies aimed at reducing CDI recurrence.

Disclosures:
Hisham Hussan, MD1, Saleh Al-Juburi, BS2, Sean K. Romeo, BS1, Mohamed Ali, MD1, Hazem Shamseddeen, MD1, Kelci Coe, MPH3, ChienWei Chiang, PhD4, Erica Reed, PharmD3. P1588 - Risk Factors for Fecal Microbiota Transplant Failure and Their Utility in Predicting FMT Outcomes: A Nationwide Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California Davis, Sacramento, CA; 2Wayne State University School of Medicine, Folsom, CA; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4College of Medicine, The Ohio State University, Columbus, OH
Introduction: C. difficile is one of the most common causes of healthcare-associated infection, often complicated by recurrent or severe C. difficile infections (CDI). Fecal microbiota transplant (FMT) is a well-established and effective treatment for recalcitrant CDI. However, not all patients successfully resolve CDI after FMT – a challenging clinical outcome. As CDI rates continue to rise, we investigated risk factors and predictors of FMT failure.
Methods: This retrospective cohort study used the 2012-2020 MarketScan database. Using billing codes, we included adults with CDI who underwent an FMT. FMT failure was defined as recurrent CDI requiring antibiotics within 6 months after FMT. Patient demographics and multiple variables including inflammatory bowel disease (IBD) were compared (Table 1). A multivariable logistic regression (MLR) model was performed to assess the relationship between our covariates and FMT outcome. We included variables in the MLR model if they were statistically significant at the univariate level. A forward selection method was conducted, which took into consideration adjusted R2, AIC, and the log-likelihood to determine the best model fit. Statistical significance was defined as a p< 0.05.
Results: Our FMT cohort included 1,126 adults (mean age of 58 years, 63% females), of which 207 (18.3%) had a failed FMT. Compared to FMT success, adults with FMT failure had higher odds of being older, females, with more comorbidities, and four-fold higher odds of co-existing IBD (P< 0.0001). Outpatient vs. inpatient FMT and FMT delivery method (colonoscopy vs. other) were also associated with 4-fold and 8-fold higher odds of FMT failure, respectively (p< 0.0001). In contrast, a history of bariatric surgery was associated with 80% lower odds of FMT failure (p< 0.001). Immunosuppression, body mass index categories, pregnancy, malignancy, and prior CDI number were not associated with our FMT outcomes. In the final MLR model, age [odds ratio (OR) 1.022; 95%CI,1.01-1.03], male sex (OR 0.65; 95% CI, 0.45-0.94), IBD (OR 2.92; 95% CI, 2.01-4.2), and FMT delivery method (OR 3.03; 95%CI, 2.15-4.28) were predictive of future FMT outcomes. Other variables were not significant on the MLR. Fig. 1 illustrates our MLR model's diagnostic ability.
Discussion: In this nationwide study, we suggest that age, sex, IBD, and FMT method can predict adults who will have an FMT failure. This data is critical for patient counseling, clinical decision-making, and future studies aimed at reducing CDI recurrence.

Figure: Fig. 1. The Receiver Operator Characteristic (ROC) of the final MLR prediction model.
Disclosures:
Hisham Hussan indicated no relevant financial relationships.
Saleh Al-Juburi indicated no relevant financial relationships.
Sean Romeo indicated no relevant financial relationships.
Mohamed Ali indicated no relevant financial relationships.
Hazem Shamseddeen indicated no relevant financial relationships.
Kelci Coe indicated no relevant financial relationships.
ChienWei Chiang indicated no relevant financial relationships.
Erica Reed indicated no relevant financial relationships.
Hisham Hussan, MD1, Saleh Al-Juburi, BS2, Sean K. Romeo, BS1, Mohamed Ali, MD1, Hazem Shamseddeen, MD1, Kelci Coe, MPH3, ChienWei Chiang, PhD4, Erica Reed, PharmD3. P1588 - Risk Factors for Fecal Microbiota Transplant Failure and Their Utility in Predicting FMT Outcomes: A Nationwide Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
