Monday Poster Session
Category: Colon
P1615 - Colorectal Cancer Screening Behaviors Among US Adults With Depression and Anxiety
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Gregory L. Riley, II, MD
Howard University
Washington, DC
Presenting Author(s)
Gregory Riley, MD1, Laiyemo Adeyinka, MD, MPH, FACG2
1Howard University, Washington, DC; 2Howard University Hospital, Washington, DC
Introduction: Individuals who are diagnosed with colorectal cancer (CRC) are often noted to have mental health disorders, particularly anxiety and depression. They are also more likely to have decreased quality of life and increased mortality from CRC. It is uncertain whether the mental illnesses reported is due to the cancer diagnosis itself, or an increased cancer risk among those with pre-existing mental illness. This is because literature has illustrated that individuals with depression/anxiety may have negative perceptions and decreased utilization of preventive services such as immunizations, dental exams, and annual checkups. The effect of depression/anxiety on CRC screening uptake is unknown.
Aim: To evaluate the relationship between depression and anxiety and colorectal cancer screening uptake among adults in the United States.
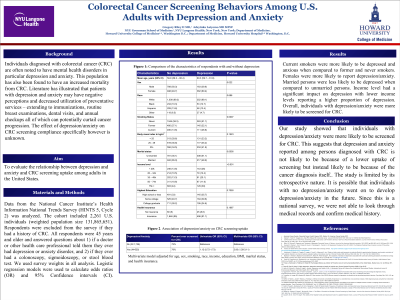
Methods: Data from the National Cancer Institute’s Health Information National Trends Survey (HINTS 5, Cycle 2) was analyzed. The analytic cohort included 2,261 U.S. adults (weighted population size = 131,865,651) who were 45 years and older and did not have a personal history of CRC. The included respondents answered questions about 1) if a doctor or other health care professional told them they ever had depression or anxiety disorder, and 2) if they ever had a colonoscopy, sigmoidoscopy, or stool test to check for CRC. We used survey weights in all analyses. Logistic regression models were used to calculate odds ratios (OR) and 95% Confidence intervals (CI).
Results: A total of 525 adults (weighted population size = 30,618,959) reported depression/anxiety. This consisted of 39.6% males and 60.4% females. Females were more likely to report depression/anxiety (p = 0.02). Current smokers were more likely to be depressed and anxious when compared to former and never smokers (p < 0.001). Furthermore, respondents who reported lower income levels had higher prevalence of depression (p < 0.001). However, married persons were less likely to be depressed when compared to unmarried persons (p < 0.001). Overall, individuals with depression/anxiety were more likely to be screened for CRC: OR = 2.00; 95% CI 1.28–3.11 (Table 1).
Discussion: Individuals with depression/anxiety were more likely to be screened for CRC. This suggests that depression and anxiety reported among persons diagnosed with CRC is probably due to the cancer diagnosis itself and not necessarily due to a lower uptake of screening among those with pre-existing mental illness.
Disclosures:
Gregory Riley, MD1, Laiyemo Adeyinka, MD, MPH, FACG2. P1615 - Colorectal Cancer Screening Behaviors Among US Adults With Depression and Anxiety, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Howard University, Washington, DC; 2Howard University Hospital, Washington, DC
Introduction: Individuals who are diagnosed with colorectal cancer (CRC) are often noted to have mental health disorders, particularly anxiety and depression. They are also more likely to have decreased quality of life and increased mortality from CRC. It is uncertain whether the mental illnesses reported is due to the cancer diagnosis itself, or an increased cancer risk among those with pre-existing mental illness. This is because literature has illustrated that individuals with depression/anxiety may have negative perceptions and decreased utilization of preventive services such as immunizations, dental exams, and annual checkups. The effect of depression/anxiety on CRC screening uptake is unknown.
Aim: To evaluate the relationship between depression and anxiety and colorectal cancer screening uptake among adults in the United States.
Methods: Data from the National Cancer Institute’s Health Information National Trends Survey (HINTS 5, Cycle 2) was analyzed. The analytic cohort included 2,261 U.S. adults (weighted population size = 131,865,651) who were 45 years and older and did not have a personal history of CRC. The included respondents answered questions about 1) if a doctor or other health care professional told them they ever had depression or anxiety disorder, and 2) if they ever had a colonoscopy, sigmoidoscopy, or stool test to check for CRC. We used survey weights in all analyses. Logistic regression models were used to calculate odds ratios (OR) and 95% Confidence intervals (CI).
Results: A total of 525 adults (weighted population size = 30,618,959) reported depression/anxiety. This consisted of 39.6% males and 60.4% females. Females were more likely to report depression/anxiety (p = 0.02). Current smokers were more likely to be depressed and anxious when compared to former and never smokers (p < 0.001). Furthermore, respondents who reported lower income levels had higher prevalence of depression (p < 0.001). However, married persons were less likely to be depressed when compared to unmarried persons (p < 0.001). Overall, individuals with depression/anxiety were more likely to be screened for CRC: OR = 2.00; 95% CI 1.28–3.11 (Table 1).
Discussion: Individuals with depression/anxiety were more likely to be screened for CRC. This suggests that depression and anxiety reported among persons diagnosed with CRC is probably due to the cancer diagnosis itself and not necessarily due to a lower uptake of screening among those with pre-existing mental illness.
Disclosures:
Gregory Riley indicated no relevant financial relationships.
Laiyemo Adeyinka indicated no relevant financial relationships.
Gregory Riley, MD1, Laiyemo Adeyinka, MD, MPH, FACG2. P1615 - Colorectal Cancer Screening Behaviors Among US Adults With Depression and Anxiety, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
