Monday Poster Session
Category: Colon
P1641 - Acute Colonic Pseudo-Obstruction After Bupropion Overdose
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Samantha Rubin, DO
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Samantha Rubin, DO, Matthew Ballenberger, MD
Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Bupropion is a widely prescribed antidepressant that acts by inhibiting the reuptake of dopamine and norepinephrine, and by antagonizing the nicotinic acetylcholine receptor. At high doses it can cause various effects including nausea, vomiting, and constipation. Severe toxic doses can lead to seizures, intestinal perforation, and ventricular dysrhythmias. While its safety profile is generally favorable, we present a rare effect of acute colonic pseudo-obstruction.
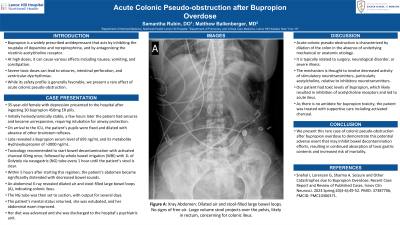
Case Description/Methods: A 35-year-old female with a history of depression presented to the hospital after ingesting 30 bupropion 450mg ER pills. Initially hemodynamically stable, a few hours later the patient had seizures and became unresponsive, requiring intubation for airway protection. On arrival to the ICU, the patient’s pupils were fixed and dilated with absence of other brainstem reflexes. Laboratory tests revealed a Bupropion serum level of 695 ng/mL and its metabolite Hydroxybupropion of >3000 ng/mL. Toxicology recommended to start bowel decontamination with activated charcoal 60mg once, followed by whole bowel irrigation (WBI) with 1L of Golytely via nasogastric (NG) tube every one hour until the patient’s stool is clear. Within five hours after starting this regimen, the patient’s abdomen became significantly distended with decreased bowel sounds. An abdominal X-ray revealed dilated air and stool-filled large bowel loops (A), indicating colonic ileus. The NG tube was then set to suction, with output for several days. The patient’s mental status returned, her abdominal exam improved, and she was extubated. Her diet was advanced and she was discharged to the hospital’s psychiatric unit.
Discussion: Acute colonic pseudo-obstruction is characterized by dilation of the colon in the absence of underlying mechanical or anatomic etiology. It is typically related to surgery, neurological disorder, or severe illness. The mechanism is thought to involve decreased activity of stimulatory neurotransmitters, particularly acetylcholine, relative to inhibitory neurotransmitters. Our patient had toxic levels of Bupropion, which likely resulted in inhibition of acetylcholine receptors and led to acute ileus. As there is no antidote for bupropion toxicity, the patient was treated with supportive care including activated charcoal. We present this rare case to demonstrate this potential adverse event which may inhibit bowel decontamination efforts, resulting in continued absorption of toxic gastric contents and increased risk of mortality.

Disclosures:
Samantha Rubin, DO, Matthew Ballenberger, MD. P1641 - Acute Colonic Pseudo-Obstruction After Bupropion Overdose, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Bupropion is a widely prescribed antidepressant that acts by inhibiting the reuptake of dopamine and norepinephrine, and by antagonizing the nicotinic acetylcholine receptor. At high doses it can cause various effects including nausea, vomiting, and constipation. Severe toxic doses can lead to seizures, intestinal perforation, and ventricular dysrhythmias. While its safety profile is generally favorable, we present a rare effect of acute colonic pseudo-obstruction.
Case Description/Methods: A 35-year-old female with a history of depression presented to the hospital after ingesting 30 bupropion 450mg ER pills. Initially hemodynamically stable, a few hours later the patient had seizures and became unresponsive, requiring intubation for airway protection. On arrival to the ICU, the patient’s pupils were fixed and dilated with absence of other brainstem reflexes. Laboratory tests revealed a Bupropion serum level of 695 ng/mL and its metabolite Hydroxybupropion of >3000 ng/mL. Toxicology recommended to start bowel decontamination with activated charcoal 60mg once, followed by whole bowel irrigation (WBI) with 1L of Golytely via nasogastric (NG) tube every one hour until the patient’s stool is clear. Within five hours after starting this regimen, the patient’s abdomen became significantly distended with decreased bowel sounds. An abdominal X-ray revealed dilated air and stool-filled large bowel loops (A), indicating colonic ileus. The NG tube was then set to suction, with output for several days. The patient’s mental status returned, her abdominal exam improved, and she was extubated. Her diet was advanced and she was discharged to the hospital’s psychiatric unit.
Discussion: Acute colonic pseudo-obstruction is characterized by dilation of the colon in the absence of underlying mechanical or anatomic etiology. It is typically related to surgery, neurological disorder, or severe illness. The mechanism is thought to involve decreased activity of stimulatory neurotransmitters, particularly acetylcholine, relative to inhibitory neurotransmitters. Our patient had toxic levels of Bupropion, which likely resulted in inhibition of acetylcholine receptors and led to acute ileus. As there is no antidote for bupropion toxicity, the patient was treated with supportive care including activated charcoal. We present this rare case to demonstrate this potential adverse event which may inhibit bowel decontamination efforts, resulting in continued absorption of toxic gastric contents and increased risk of mortality.

Figure: Xray Abdomen showing dilated air and stool-filled large bowel loops. No signs of free air. Findings indicate colonic ileus.
Disclosures:
Samantha Rubin indicated no relevant financial relationships.
Matthew Ballenberger indicated no relevant financial relationships.
Samantha Rubin, DO, Matthew Ballenberger, MD. P1641 - Acute Colonic Pseudo-Obstruction After Bupropion Overdose, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
