Monday Poster Session
Category: Colon
P1670 - Ischemic Colitis Presenting With Painless Hematochezia: The Stripe Sign
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- CB
Christopher Bouvette, MD
University of Oklahoma College of Medicine
Oklahoma City, Oklahoma
Presenting Author(s)
Christopher Bouvette, MD1, Ahmad Basil Nasir, MD1, Jalal Gondal, BA1, Tokunbo Ajayi, MD1, Donald Kastens, MD2
1University of Oklahoma College of Medicine, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma CIty, OK
Introduction: Ischemic colitis can be seen with arterial or venous occlusive and nonocclusive etiologies and is typically manifest by painful hematochezia. Risk factors include atherosclerotic disease, hypotension, thromboembolic events, and iatrogenic. Here we describe a case of extensive ischemic colitis uniquely manifest by painless hematochezia.
Case Description/Methods: We present an 80-year old male with history of atrial fibrillation (on apixaban), hypertension, and prior remote open abdominal aortic aneurysm repair admitted for syncope. GI was consulted for hematochezia. Upon arrival, the patient was awake and oriented. Blood pressure was 138/105 and telemetry showed atrial fibrillation with rapid ventricular response. His abdomen was soft and nontender to palpation in all quadrants. Digital rectal exam revealed bright red blood with clots. Labs showed: WBC 8.0 K/mm3, Hgb 12.9 g/dL, Plt 268 K/mm3, BUN 22 mg/dL, creatinine 1.82 mg/dL, and lactic acid 2.5 mM/L. Colonoscopy demonstrated a diffuse area of severely friable and dusky mucosa in the sigmoid colon, and an evident stripe sign extending proximally to the splenic flexure. Biopsy histology was entirely consistent with ischemic colitis. Given prior aortic aneurysm repair and extensive ischemia, abdominal computed angiography was obtained. This revealed near total atherosclerotic occlusion of the proximal inferior mesenteric artery. The patient was provided supportive care and recovered well, eventually tolerating apixaban prior to discharge.
Discussion: Ischemic colitis is typically characterized by onset of crampy abdominal pain out of proportion to abdominal exam, with subsequent urgency and hematochezia. In those with atherosclerotic burden relative hypoperfusion progresses over time effectively lowering patient reserve. Aortic aneurysm repair often involves sacrifice of the middle sacral artery and can be complicated by perioperative or post-procedural ischemia. Despite this atypical painless presentation, the case demonstrates classical endoscopic findings of ischemic colitis, including a very lengthy stripe sign. We suspect atrial fibrillation with rapid ventricular response to have contributed to a picture of cardiac syncope yielding IMA distribution ischemic colitis in the setting of significant atherosclerotic burden.

Disclosures:
Christopher Bouvette, MD1, Ahmad Basil Nasir, MD1, Jalal Gondal, BA1, Tokunbo Ajayi, MD1, Donald Kastens, MD2. P1670 - Ischemic Colitis Presenting With Painless Hematochezia: The Stripe Sign, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Oklahoma College of Medicine, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma CIty, OK
Introduction: Ischemic colitis can be seen with arterial or venous occlusive and nonocclusive etiologies and is typically manifest by painful hematochezia. Risk factors include atherosclerotic disease, hypotension, thromboembolic events, and iatrogenic. Here we describe a case of extensive ischemic colitis uniquely manifest by painless hematochezia.
Case Description/Methods: We present an 80-year old male with history of atrial fibrillation (on apixaban), hypertension, and prior remote open abdominal aortic aneurysm repair admitted for syncope. GI was consulted for hematochezia. Upon arrival, the patient was awake and oriented. Blood pressure was 138/105 and telemetry showed atrial fibrillation with rapid ventricular response. His abdomen was soft and nontender to palpation in all quadrants. Digital rectal exam revealed bright red blood with clots. Labs showed: WBC 8.0 K/mm3, Hgb 12.9 g/dL, Plt 268 K/mm3, BUN 22 mg/dL, creatinine 1.82 mg/dL, and lactic acid 2.5 mM/L. Colonoscopy demonstrated a diffuse area of severely friable and dusky mucosa in the sigmoid colon, and an evident stripe sign extending proximally to the splenic flexure. Biopsy histology was entirely consistent with ischemic colitis. Given prior aortic aneurysm repair and extensive ischemia, abdominal computed angiography was obtained. This revealed near total atherosclerotic occlusion of the proximal inferior mesenteric artery. The patient was provided supportive care and recovered well, eventually tolerating apixaban prior to discharge.
Discussion: Ischemic colitis is typically characterized by onset of crampy abdominal pain out of proportion to abdominal exam, with subsequent urgency and hematochezia. In those with atherosclerotic burden relative hypoperfusion progresses over time effectively lowering patient reserve. Aortic aneurysm repair often involves sacrifice of the middle sacral artery and can be complicated by perioperative or post-procedural ischemia. Despite this atypical painless presentation, the case demonstrates classical endoscopic findings of ischemic colitis, including a very lengthy stripe sign. We suspect atrial fibrillation with rapid ventricular response to have contributed to a picture of cardiac syncope yielding IMA distribution ischemic colitis in the setting of significant atherosclerotic burden.

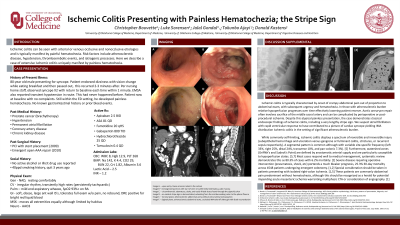
Figure: Figure 1.
Image A. – Upon entry, linear erosions noted in the rectum.
Image B. – Circumferential, edematous, dusky, and easily friable tissue found through the sigmoid colon.
Image C. – An evident stripe sign is demonstrated, extending from the mid-descending colon to the splenic flexure.
Image A. – Upon entry, linear erosions noted in the rectum.
Image B. – Circumferential, edematous, dusky, and easily friable tissue found through the sigmoid colon.
Image C. – An evident stripe sign is demonstrated, extending from the mid-descending colon to the splenic flexure.
Disclosures:
Christopher Bouvette indicated no relevant financial relationships.
Ahmad Basil Nasir indicated no relevant financial relationships.
Jalal Gondal indicated no relevant financial relationships.
Tokunbo Ajayi indicated no relevant financial relationships.
Donald Kastens indicated no relevant financial relationships.
Christopher Bouvette, MD1, Ahmad Basil Nasir, MD1, Jalal Gondal, BA1, Tokunbo Ajayi, MD1, Donald Kastens, MD2. P1670 - Ischemic Colitis Presenting With Painless Hematochezia: The Stripe Sign, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
