Monday Poster Session
Category: Colon
P1674 - Rare Dysplastic Transformation of a Hamartomatous Polyp in a Patient With Peutz-Jeghers Syndrome
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Emily Minor, MD, PhD
University of Virginia
Charlottesville, VA
Presenting Author(s)
Emily Minor, MD, PhD, Christy Gilman, MD, MS, Kyle A. Hodge, MD, Christopher Moskaluk, MD, PhD, Andrew P. Copland, MD
University of Virginia, Charlottesville, VA
Introduction: Peutz-Jeghers syndrome (PJS) is an autosomal dominant condition characterized by mucocutaneous pigmentation and the development of hamartomatous polyps throughout the gastrointestinal tract. There are no major distinguishing characteristics endoscopically, but histologically, hamartomas contain a proliferation of smooth muscle that extends into the lamina propria. The smooth muscle core and absence of dysplasia are defining characteristics, though very rarely dysplasia does occur.
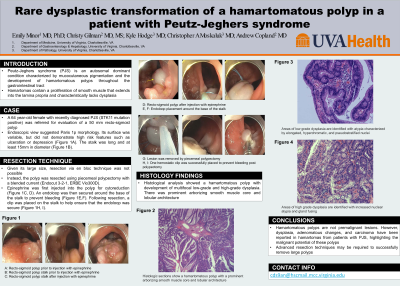
Case Description/Methods: A 64 year-old female with recently diagnosed PJS (STK11 mutation) was referred for evaluation of a 50 mm recto-sigmoid polyp. Endoscopic view suggested Paris 1p morphology with a variable surface, but no high-risk features such as ulceration or depression (Figure 1A). The stalk was long and at least 15mm in diameter (Figure 1B). To help cytoreduce the polyp, epinephrine was injected into the polyp (Figure 1C, D). An endoloop was secured around the base of the stalk to prevent bleeding (Figure 1E, F). We were unsuccessful in encircling the polyp with a 33mm snare, so instead the lesion was removed by piecemeal polypectomy (Figure 1G) using a blended current (Endocut 3-2-1, ERBE Vio300D). After debulking, we resected the remaining polyp and the stalk just above the endoloop (Figure 1H). The resected stalk was sent in a separate jar to facilitate histologic assessment of the stalk margin. A clip was placed on the stalk to prevent bleeding after polypectomy (Figure 1I).
Histological analysis showed a hamartomatous polyp with development of multifocal low-grade and high-grade dysplasia. There was prominent arborizing smooth muscle core and lobular architecture (Figure 2). Areas of low grade dysplasia were identified with atypia characterized by elongated, hyperchromatic and pseudostratified nuclei (Figure 3). Areas of high grade dysplasia were identified with increased nuclear atypia and gland fusing (Figure 4). Additional polyps were removed and the patient was scheduled for follow-up endoscopy, but she ultimately passed away from other complications.
Discussion: Hamartomatous polyps are not premalignant lesions however, dysplasia, adenomatous changes and carcinoma in hamartomatous polyps have been reported in patients with PJS. This case supports previous reports of potential malignant transformation of Peutz-Jeghers hamartomatous polyps and highlights an approach to removing large hamartomatous polyps where the lesion is too large to perform en bloc resection with conventional techniques.

Disclosures:
Emily Minor, MD, PhD, Christy Gilman, MD, MS, Kyle A. Hodge, MD, Christopher Moskaluk, MD, PhD, Andrew P. Copland, MD. P1674 - Rare Dysplastic Transformation of a Hamartomatous Polyp in a Patient With Peutz-Jeghers Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Virginia, Charlottesville, VA
Introduction: Peutz-Jeghers syndrome (PJS) is an autosomal dominant condition characterized by mucocutaneous pigmentation and the development of hamartomatous polyps throughout the gastrointestinal tract. There are no major distinguishing characteristics endoscopically, but histologically, hamartomas contain a proliferation of smooth muscle that extends into the lamina propria. The smooth muscle core and absence of dysplasia are defining characteristics, though very rarely dysplasia does occur.
Case Description/Methods: A 64 year-old female with recently diagnosed PJS (STK11 mutation) was referred for evaluation of a 50 mm recto-sigmoid polyp. Endoscopic view suggested Paris 1p morphology with a variable surface, but no high-risk features such as ulceration or depression (Figure 1A). The stalk was long and at least 15mm in diameter (Figure 1B). To help cytoreduce the polyp, epinephrine was injected into the polyp (Figure 1C, D). An endoloop was secured around the base of the stalk to prevent bleeding (Figure 1E, F). We were unsuccessful in encircling the polyp with a 33mm snare, so instead the lesion was removed by piecemeal polypectomy (Figure 1G) using a blended current (Endocut 3-2-1, ERBE Vio300D). After debulking, we resected the remaining polyp and the stalk just above the endoloop (Figure 1H). The resected stalk was sent in a separate jar to facilitate histologic assessment of the stalk margin. A clip was placed on the stalk to prevent bleeding after polypectomy (Figure 1I).
Histological analysis showed a hamartomatous polyp with development of multifocal low-grade and high-grade dysplasia. There was prominent arborizing smooth muscle core and lobular architecture (Figure 2). Areas of low grade dysplasia were identified with atypia characterized by elongated, hyperchromatic and pseudostratified nuclei (Figure 3). Areas of high grade dysplasia were identified with increased nuclear atypia and gland fusing (Figure 4). Additional polyps were removed and the patient was scheduled for follow-up endoscopy, but she ultimately passed away from other complications.
Discussion: Hamartomatous polyps are not premalignant lesions however, dysplasia, adenomatous changes and carcinoma in hamartomatous polyps have been reported in patients with PJS. This case supports previous reports of potential malignant transformation of Peutz-Jeghers hamartomatous polyps and highlights an approach to removing large hamartomatous polyps where the lesion is too large to perform en bloc resection with conventional techniques.

Figure: Figure 1:
A. Recto-sigmoid polyp prior to injection with epinephrine
B. Recto-sigmoid polyp stalk prior to injection with epinephrine
C. Recto-sigmoid polyp stalk after injection with epinephrine
D. Recto-sigmoid polyp after injection with epinephrine
E. Endoloop placement around the base of the stalk
F. Endoloop placement around the base of the stalk
G. Lesion was removed by piecemeal polypectomy
H. One hemostatic clip was successfully placed to prevent bleeding post polypectomy
I. One hemostatic clip was successfully placed to prevent bleeding post polypectomy
Figure 2: Arborizing smooth muscle core and lobular architecture
Figure 3: Areas of low grade dysplasia
Figure 4: Areas of high grade dysplasia
A. Recto-sigmoid polyp prior to injection with epinephrine
B. Recto-sigmoid polyp stalk prior to injection with epinephrine
C. Recto-sigmoid polyp stalk after injection with epinephrine
D. Recto-sigmoid polyp after injection with epinephrine
E. Endoloop placement around the base of the stalk
F. Endoloop placement around the base of the stalk
G. Lesion was removed by piecemeal polypectomy
H. One hemostatic clip was successfully placed to prevent bleeding post polypectomy
I. One hemostatic clip was successfully placed to prevent bleeding post polypectomy
Figure 2: Arborizing smooth muscle core and lobular architecture
Figure 3: Areas of low grade dysplasia
Figure 4: Areas of high grade dysplasia
Disclosures:
Emily Minor indicated no relevant financial relationships.
Christy Gilman indicated no relevant financial relationships.
Kyle Hodge indicated no relevant financial relationships.
Christopher Moskaluk indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Emily Minor, MD, PhD, Christy Gilman, MD, MS, Kyle A. Hodge, MD, Christopher Moskaluk, MD, PhD, Andrew P. Copland, MD. P1674 - Rare Dysplastic Transformation of a Hamartomatous Polyp in a Patient With Peutz-Jeghers Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
