Monday Poster Session
Category: Colon
P1735 - Classification and Locoregional Treatment of Rectal Neuroendocrine Tumors
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- GS
Gurdeep Singh, DO
AdventHealth
Orlando, FL
Presenting Author(s)
Gurdeep Singh, DO, Arooj Mian, MD, Mehreen Ali, MD, Swotantra Gautam, MD, Baha Fawwaz, MD, Aimen Farooq, MD
AdventHealth, Orlando, FL
Introduction: Gastrointestinal neuroendocrine neoplasms (NENs) are a rare clinical entity that arise from dysregulated proliferation of neuroendocrine cells in the digestive tract. The World Health Organization has subdivided NENs into neuroendocrine tumors (NETs) and neuroendocrine carcinomas (NECs), with the dichotomy primarily stemming from the degree of differentiation and proliferative activity.
Case Description/Methods: A 43-year-old male with a past medical history of hypertension, obesity, and obstructive sleep apnea presented to his primary care physician’s office with complaint of painless rectal bleeding with a concomitant weight loss of 10-15 pounds and intermittent abdominal pain. Endoscopic evaluation was remarkable for a 5 mm rectal polyp roughly 10 cm from the anal verge. The polyp was resected and was determined to have staining characteristics consistent with a low grade neuroendocrine tumor. Immunostaining for synaptophysin, chromogranin, CD56, and CAM5.2 were positive, staining for CK20 was negative.
A CT scan of the abdomen/pelvis was ordered and revealed no metastatic disease. Given the absence of metastasis on radiographic and endoscopic evaluation, the patient was managed conservatively with observation. Subsequent CT scans of the abdomen/pelvis continued to remain negative for distal organ or lymphovascular metastases. The patient is presently in good health and continues to follow-up with Hematology/Oncology and Gastroenterology for periodic evaluation.
Discussion: Rectal neuroendocrine neoplasia is a rare clinical entity that arises from unchecked proliferation of neuroendocrine cells in digestive tract. Despite having an indolent clinical course, resection is recommended for all rectal neuroendocrine tumors. Locoregional endoscopic resection versus radical resection can be used for adequate tissue removal depending on the characteristics of the tumor and degree of invasion. For tumors less than 10 mm in size without high-risk features or invasion into the muscularis propria, endoscopic resection is recommended. For tumors greater than 20 mm in size, surgical resection is the mainstay of treatment. While the optimal therapy for tumors between 10 – 20 mm in size is controversial, the evidence suggests radical resection for tumors with high-risk characteristics or local invasion. Advanced endoscopic techniques like modified endoscopic mucosal resection or endoscopic submucosal dissection for en bloc resection in tumors without these features is recommended.

Disclosures:
Gurdeep Singh, DO, Arooj Mian, MD, Mehreen Ali, MD, Swotantra Gautam, MD, Baha Fawwaz, MD, Aimen Farooq, MD. P1735 - Classification and Locoregional Treatment of Rectal Neuroendocrine Tumors, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
AdventHealth, Orlando, FL
Introduction: Gastrointestinal neuroendocrine neoplasms (NENs) are a rare clinical entity that arise from dysregulated proliferation of neuroendocrine cells in the digestive tract. The World Health Organization has subdivided NENs into neuroendocrine tumors (NETs) and neuroendocrine carcinomas (NECs), with the dichotomy primarily stemming from the degree of differentiation and proliferative activity.
Case Description/Methods: A 43-year-old male with a past medical history of hypertension, obesity, and obstructive sleep apnea presented to his primary care physician’s office with complaint of painless rectal bleeding with a concomitant weight loss of 10-15 pounds and intermittent abdominal pain. Endoscopic evaluation was remarkable for a 5 mm rectal polyp roughly 10 cm from the anal verge. The polyp was resected and was determined to have staining characteristics consistent with a low grade neuroendocrine tumor. Immunostaining for synaptophysin, chromogranin, CD56, and CAM5.2 were positive, staining for CK20 was negative.
A CT scan of the abdomen/pelvis was ordered and revealed no metastatic disease. Given the absence of metastasis on radiographic and endoscopic evaluation, the patient was managed conservatively with observation. Subsequent CT scans of the abdomen/pelvis continued to remain negative for distal organ or lymphovascular metastases. The patient is presently in good health and continues to follow-up with Hematology/Oncology and Gastroenterology for periodic evaluation.
Discussion: Rectal neuroendocrine neoplasia is a rare clinical entity that arises from unchecked proliferation of neuroendocrine cells in digestive tract. Despite having an indolent clinical course, resection is recommended for all rectal neuroendocrine tumors. Locoregional endoscopic resection versus radical resection can be used for adequate tissue removal depending on the characteristics of the tumor and degree of invasion. For tumors less than 10 mm in size without high-risk features or invasion into the muscularis propria, endoscopic resection is recommended. For tumors greater than 20 mm in size, surgical resection is the mainstay of treatment. While the optimal therapy for tumors between 10 – 20 mm in size is controversial, the evidence suggests radical resection for tumors with high-risk characteristics or local invasion. Advanced endoscopic techniques like modified endoscopic mucosal resection or endoscopic submucosal dissection for en bloc resection in tumors without these features is recommended.

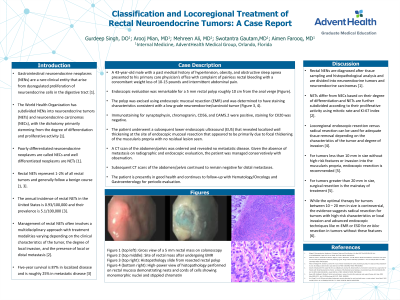
Figure: A: Histopathology of resected rectal polyp showing mucosal glands overlying the submucosal carcinoid tumor
B: High-power view showing nests and cords of cells with monomorphic nuclei and stippled chromatin
C; Immunohistochemical staining of slide demonstrating positivity to synaptophysin
D: Positive immunohistochemical staining for chromogranin
B: High-power view showing nests and cords of cells with monomorphic nuclei and stippled chromatin
C; Immunohistochemical staining of slide demonstrating positivity to synaptophysin
D: Positive immunohistochemical staining for chromogranin
Disclosures:
Gurdeep Singh indicated no relevant financial relationships.
Arooj Mian indicated no relevant financial relationships.
Mehreen Ali indicated no relevant financial relationships.
Swotantra Gautam indicated no relevant financial relationships.
Baha Fawwaz indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Gurdeep Singh, DO, Arooj Mian, MD, Mehreen Ali, MD, Swotantra Gautam, MD, Baha Fawwaz, MD, Aimen Farooq, MD. P1735 - Classification and Locoregional Treatment of Rectal Neuroendocrine Tumors, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
