Monday Poster Session
Category: Colorectal Cancer Prevention
P1761 - Characterization of Colorectal Cancer Screening Rates in Food Insecure Individuals Using a Nationally Representative Survey
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Olivia Jordan, MD
University of California, Los Angeles
Los Angeles, CA
Presenting Author(s)
Olivia Jordan, MD1, Yvonne Lei, BA2, Jayraan Badiee, MPH1, Folasade P.. May, MD, PhD, MPhil3
1University of California, Los Angeles, Los Angeles, CA; 2David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 3UCLA Health, Los Angeles, CA
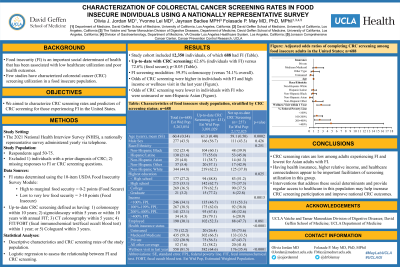
Introduction: Food insecurity (FI) is an important social determinant of health that has been associated with low healthcare utilization and poor health outcomes. Few studies have characterized colorectal cancer (CRC) screening utilization in a food insecure population. We aimed to characterize CRC screening rates and predictors of CRC screening for those experiencing FI in the United States.
Methods: We used data from the 2021 National Health Interview Survey (NHIS). We included individuals aged 50-75 and excluded individuals with a prior diagnosis of CRC or missing responses to food insecurity or CRC screening questions. FI status was determined using the USDA Adult Food Security Module in which FI is defined as having low or very low food security. We characterized screened respondents as those who had a colonoscopy within 10 years, sigmoidoscopy within 5 years, CT colonography within 5 years, FIT/FOBT within 1 year, or Cologuard within 3 years. We calculated descriptive characteristics and screening rates of the study population and performed a logistic regression to assess the relationship between patient factors and CRC screening.
Results: Our study included 688 individuals who identified as food insecure. 62.6% were screened for CRC (compared to 72.6% for food secure respondents). The average age was 60.4 years; 44.8% were non-Hispanic White and 23.4% were non-Hispanic Black. CRC screening rates were lowest for non-Hispanic Asian respondents (38.7%). Invasive tests were more common than home-based screening modalities; 59.5% underwent colonoscopy. For all racial/ethnic groups, FIT/FOBT and colonoscopy were the most common home-based and invasive screening modalities, respectively. In a controlled model, odds of CRC screening were significantly higher in FI individuals who had attained higher income levels and who had a wellness visit in the last year (Table 1). Odds of screening were significantly lower for FI individuals who were uninsured or non-Hispanic Asian.
Discussion: CRC screening rates are low among food insecure adults and lowest for Asian adults with FI. Having health insurance, higher relative income, and healthcare connectedness appear to be important facilitators of screening utilization in this group. Our findings suggest that interventions that aim to address these social determinants and provide regular access to healthcare in this vulnerable group may help increase low CRC screening participation and improve national CRC outcomes.
Disclosures:
Olivia Jordan, MD1, Yvonne Lei, BA2, Jayraan Badiee, MPH1, Folasade P.. May, MD, PhD, MPhil3. P1761 - Characterization of Colorectal Cancer Screening Rates in Food Insecure Individuals Using a Nationally Representative Survey, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California, Los Angeles, Los Angeles, CA; 2David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 3UCLA Health, Los Angeles, CA
Introduction: Food insecurity (FI) is an important social determinant of health that has been associated with low healthcare utilization and poor health outcomes. Few studies have characterized colorectal cancer (CRC) screening utilization in a food insecure population. We aimed to characterize CRC screening rates and predictors of CRC screening for those experiencing FI in the United States.
Methods: We used data from the 2021 National Health Interview Survey (NHIS). We included individuals aged 50-75 and excluded individuals with a prior diagnosis of CRC or missing responses to food insecurity or CRC screening questions. FI status was determined using the USDA Adult Food Security Module in which FI is defined as having low or very low food security. We characterized screened respondents as those who had a colonoscopy within 10 years, sigmoidoscopy within 5 years, CT colonography within 5 years, FIT/FOBT within 1 year, or Cologuard within 3 years. We calculated descriptive characteristics and screening rates of the study population and performed a logistic regression to assess the relationship between patient factors and CRC screening.
Results: Our study included 688 individuals who identified as food insecure. 62.6% were screened for CRC (compared to 72.6% for food secure respondents). The average age was 60.4 years; 44.8% were non-Hispanic White and 23.4% were non-Hispanic Black. CRC screening rates were lowest for non-Hispanic Asian respondents (38.7%). Invasive tests were more common than home-based screening modalities; 59.5% underwent colonoscopy. For all racial/ethnic groups, FIT/FOBT and colonoscopy were the most common home-based and invasive screening modalities, respectively. In a controlled model, odds of CRC screening were significantly higher in FI individuals who had attained higher income levels and who had a wellness visit in the last year (Table 1). Odds of screening were significantly lower for FI individuals who were uninsured or non-Hispanic Asian.
Discussion: CRC screening rates are low among food insecure adults and lowest for Asian adults with FI. Having health insurance, higher relative income, and healthcare connectedness appear to be important facilitators of screening utilization in this group. Our findings suggest that interventions that aim to address these social determinants and provide regular access to healthcare in this vulnerable group may help increase low CRC screening participation and improve national CRC outcomes.
Disclosures:
Olivia Jordan indicated no relevant financial relationships.
Yvonne Lei indicated no relevant financial relationships.
Jayraan Badiee indicated no relevant financial relationships.
Folasade May: Exact Sciences – Consultant, Grant/Research Support. Freenome – Consultant. Geneoscopy – Consultant.
Olivia Jordan, MD1, Yvonne Lei, BA2, Jayraan Badiee, MPH1, Folasade P.. May, MD, PhD, MPhil3. P1761 - Characterization of Colorectal Cancer Screening Rates in Food Insecure Individuals Using a Nationally Representative Survey, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
