Monday Poster Session
Category: Colorectal Cancer Prevention
P1772 - Surveillance Colonoscopy After Endoscopic Resection of Large Laterally Spreading Tumors (≥20 mm) Detects High-Risk Synchronous Lesions
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Paul P. Shao, MD
Stanford University
Redwood City, CA
Presenting Author(s)
Award: Outstanding Research Award in the Colorectal Cancer Prevention Category (Trainee)
Award: Presidential Poster Award
Paul P. Shao, MD1, Wassem Juakiem, MD2, Leila Neshatian, MD, MSc3, Samer El-Dika, MD4
1Stanford University, Redwood City, CA; 281st Medical Group, Keesler Medical Center, Biloxi, MS; 3Stanford, Redwood City, CA; 4Stanford University, Palo Alto, CA
Introduction: Patients with large laterally spreading tumors (adenomas ≥20 mm) are at increased risk for interval cancers. Current guidelines recommend surveillance colonoscopy within 6 months only after piecemeal endoscopic resection of lesions ≥20 mm to evaluate resection sites for local recurrence. Outcomes of surveillance colonoscopy in this high-risk population is largely unknown. The aim of this study was to determine the rate and characteristics of missed synchronous lesions in patients who underwent endoscopic resection of large laterally spreading tumors (LLSTs).
Methods: This is a retrospective cohort study that included adult patients who were referred to a tertiary center for endoscopic resection of LLSTs (≥20 mm) from January 2017 to May 2022. To be included in the analysis, patients must have had a follow up surveillance colonoscopy within 18 months of the endoscopic resection of the large polyps. Patients with history of hereditary polyposis syndromes, inflammatory bowel disease, colon cancer, and colon resection or if the index polyp is not an adenoma, or sessile serrated polyp (SSP) were excluded. Logistic regression model was used for predictive factors of missed lesions using Stata 14.
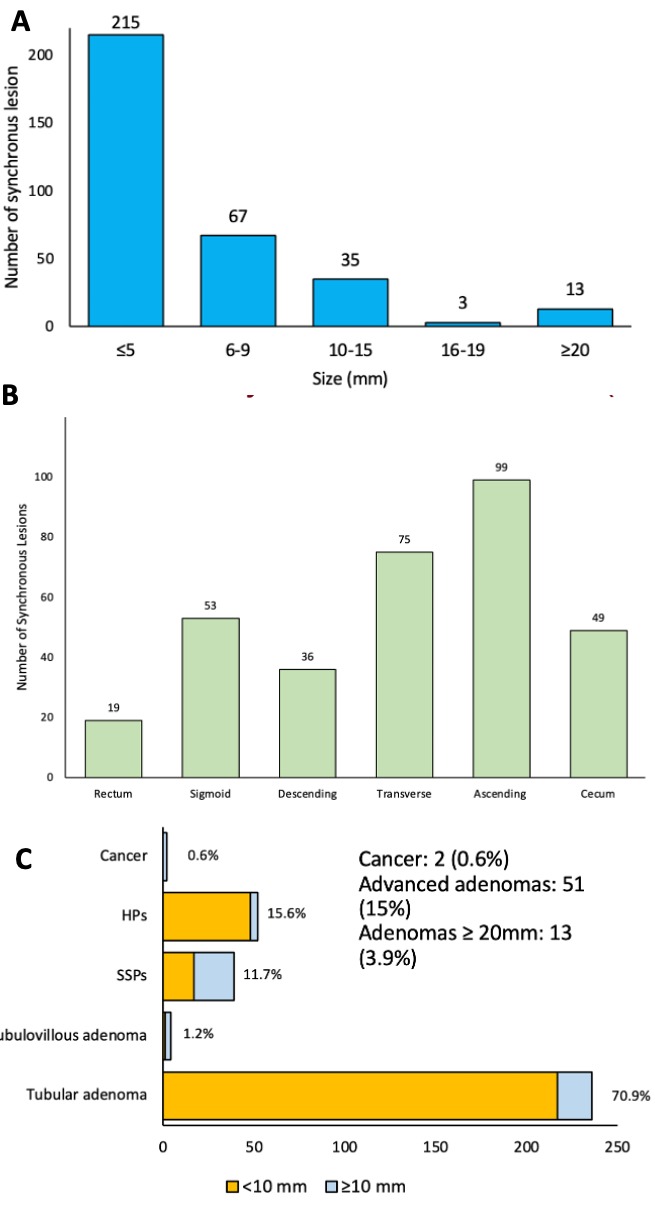
Results: Of a total of 456 patients who had undergone endoscopic resection of LLSTs, 250 patients (54.8%) had surveillance colonoscopy within 18 months. The average age was 65.5 years and 56% of the patients were male. Among them, 129 patients (51.6%) were found to have polyps on surveillance colonoscopy with a total of 333 missed lesions. 190 (57.1%) missed lesions were found proximal to the splenic flexure. The missed lesions ranged from 1 mm to 50 mm in size. 215 (64.6%) were diminutive (≤ 5mm). Most lesions were tubular adenomas (70.0%), followed by hyperplastic polyps (15.6%), SSPs (11.7%), and tubulovillous adenomas (1.2%). There were high-risk lesions, including 2 adenocarcinomas (0.6%), 51 advanced adenomas (15%) and 13 adenomas that were ≥20 mm in size (3.9%). In the multiple logistic regression analysis, we found that age was the only risk factor significantly associated with missed synchronous lesions.
Discussion: Our study highlights the significant rate of missed, high-risk synchronous lesions in patients who underwent endoscopic resection of LLSTs. Our findings underscored the importance of surveillance colonoscopy following endoscopic resection of LLSTs not only to examine resection sites for residual polyps but also to look for missed synchronous lesions.
Disclosures:
Paul P. Shao, MD1, Wassem Juakiem, MD2, Leila Neshatian, MD, MSc3, Samer El-Dika, MD4. P1772 - Surveillance Colonoscopy After Endoscopic Resection of Large Laterally Spreading Tumors (≥20 mm) Detects High-Risk Synchronous Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Award: Presidential Poster Award
Paul P. Shao, MD1, Wassem Juakiem, MD2, Leila Neshatian, MD, MSc3, Samer El-Dika, MD4
1Stanford University, Redwood City, CA; 281st Medical Group, Keesler Medical Center, Biloxi, MS; 3Stanford, Redwood City, CA; 4Stanford University, Palo Alto, CA
Introduction: Patients with large laterally spreading tumors (adenomas ≥20 mm) are at increased risk for interval cancers. Current guidelines recommend surveillance colonoscopy within 6 months only after piecemeal endoscopic resection of lesions ≥20 mm to evaluate resection sites for local recurrence. Outcomes of surveillance colonoscopy in this high-risk population is largely unknown. The aim of this study was to determine the rate and characteristics of missed synchronous lesions in patients who underwent endoscopic resection of large laterally spreading tumors (LLSTs).
Methods: This is a retrospective cohort study that included adult patients who were referred to a tertiary center for endoscopic resection of LLSTs (≥20 mm) from January 2017 to May 2022. To be included in the analysis, patients must have had a follow up surveillance colonoscopy within 18 months of the endoscopic resection of the large polyps. Patients with history of hereditary polyposis syndromes, inflammatory bowel disease, colon cancer, and colon resection or if the index polyp is not an adenoma, or sessile serrated polyp (SSP) were excluded. Logistic regression model was used for predictive factors of missed lesions using Stata 14.
Results: Of a total of 456 patients who had undergone endoscopic resection of LLSTs, 250 patients (54.8%) had surveillance colonoscopy within 18 months. The average age was 65.5 years and 56% of the patients were male. Among them, 129 patients (51.6%) were found to have polyps on surveillance colonoscopy with a total of 333 missed lesions. 190 (57.1%) missed lesions were found proximal to the splenic flexure. The missed lesions ranged from 1 mm to 50 mm in size. 215 (64.6%) were diminutive (≤ 5mm). Most lesions were tubular adenomas (70.0%), followed by hyperplastic polyps (15.6%), SSPs (11.7%), and tubulovillous adenomas (1.2%). There were high-risk lesions, including 2 adenocarcinomas (0.6%), 51 advanced adenomas (15%) and 13 adenomas that were ≥20 mm in size (3.9%). In the multiple logistic regression analysis, we found that age was the only risk factor significantly associated with missed synchronous lesions.
Discussion: Our study highlights the significant rate of missed, high-risk synchronous lesions in patients who underwent endoscopic resection of LLSTs. Our findings underscored the importance of surveillance colonoscopy following endoscopic resection of LLSTs not only to examine resection sites for residual polyps but also to look for missed synchronous lesions.
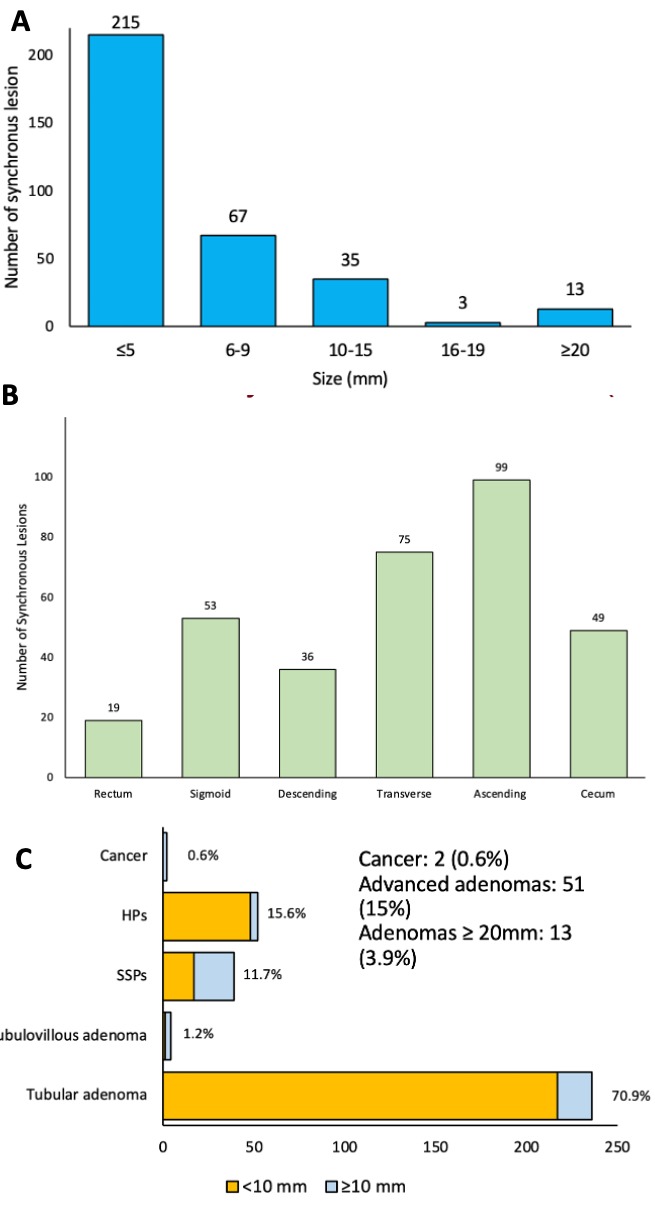
Figure: Characteristics of synchronous lesions (n=333): A. Size of synchronous lesion B. Location of synchronous lesions C. Histology of synchronous lesions
Disclosures:
Paul Shao indicated no relevant financial relationships.
Wassem Juakiem indicated no relevant financial relationships.
Leila Neshatian: salix, Ardelyx, GI supply, Vibrant – Advisory Committee/Board Member, Consultant.
Samer El-Dika indicated no relevant financial relationships.
Paul P. Shao, MD1, Wassem Juakiem, MD2, Leila Neshatian, MD, MSc3, Samer El-Dika, MD4. P1772 - Surveillance Colonoscopy After Endoscopic Resection of Large Laterally Spreading Tumors (≥20 mm) Detects High-Risk Synchronous Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


