Monday Poster Session
Category: Colorectal Cancer Prevention
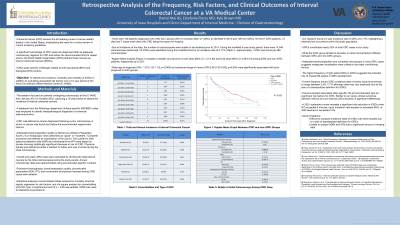
P1776 - Retrospective Analysis of the Frequency, Risk Factors, and Clinical Outcomes of Interval Colorectal Cancer at a VA Medical Center
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Daniel Mai
Roy J. and Lucille A. Carver College of Medicine
Coralville, IA
Presenting Author(s)
Daniel Mai, 1, Estefania Flores, MD2, Kyle Brown, MD2
1Roy J. and Lucille A. Carver College of Medicine, Coralville, IA; 2University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Colonoscopy is widely used to diagnose colon cancers (CRC) and remove premalignant lesions. Per literature review, CRC continues to be diagnosed after an adequate colonoscopy and prior to the recommended time for repeat exam in between 3.7% to 8.2% of cases. The goal of our study was to determine the frequency of interval colorectal cancers (iCRCs) at our center, to assess factors associated with diagnoses of iCRC, and to evaluate the effects of iCRC on patient outcomes.
Methods: We identified all patients with a histopathological diagnosis of CRC at the Iowa City VAMC for the past 10 years by searching specific SNOMED codes within the Pathology database. Interval CRC was defined as CRC diagnosed in the interval after a colonoscopy disclosed no cancer and before the recommended interval for repeat exam. Primary variables include demographics, comorbidities, stage & location of cancer, and quality of bowel preparation. Secondary variables were the length of survival after diagnosis, morbidity and mortality of iCRC patients. Kaplan Meier analysis was used to assess survival. Binomial logistic regression analysis was used to assess risk factors and poor prognosis. Chi square analysis was used to assess comorbidities and type of CRC. P-value < 0.05 was considered statistically significant.
Results: 136 patients were diagnosed with CRC over a 10-year interval. Type of CRC, mean age, and statistical significance of comorbidities are listed in the table. Right-sided CRCs were significantly more common in the group with iCRC (p=0.01). Tumor location and iCRC versus non-iCRC were not associated with prognosis (p >0.05), but older age at diagnosis (OR = 1.07 [1.02-1.12]; p=0.005) and advanced stage of cancer (OR=2.60 [1.02-6.63]; p=0.045) were significantly associated with poor prognosis. Of the 27 iCRC patients, 13 died with iCRC cited as the reason for hospice in 7. Median survival time (yrs) of iCRC and non-iCRC patients were 3.20 (95% CI 1.47-4.92) and 6.20 (95% CI 3.29-9.10), respectively (NS).
Discussion: iCRCs comprised nearly 20% of total CRC cases in this series . The iCRC group tended to be older but there were no other clinical factors that differed between the iCRC and non-iCRC groups. The quality of bowel preparation documented on the prior colonoscopies of the iCRC group was adequate in most cases, making it unlikely that inadequate visualization was a major factor. The higher frequency of right-sided CRCs in iCRCs suggests that flat polyps that were missed may contribute to iCRCs.

Disclosures:
Daniel Mai, 1, Estefania Flores, MD2, Kyle Brown, MD2. P1776 - Retrospective Analysis of the Frequency, Risk Factors, and Clinical Outcomes of Interval Colorectal Cancer at a VA Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Roy J. and Lucille A. Carver College of Medicine, Coralville, IA; 2University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Colonoscopy is widely used to diagnose colon cancers (CRC) and remove premalignant lesions. Per literature review, CRC continues to be diagnosed after an adequate colonoscopy and prior to the recommended time for repeat exam in between 3.7% to 8.2% of cases. The goal of our study was to determine the frequency of interval colorectal cancers (iCRCs) at our center, to assess factors associated with diagnoses of iCRC, and to evaluate the effects of iCRC on patient outcomes.
Methods: We identified all patients with a histopathological diagnosis of CRC at the Iowa City VAMC for the past 10 years by searching specific SNOMED codes within the Pathology database. Interval CRC was defined as CRC diagnosed in the interval after a colonoscopy disclosed no cancer and before the recommended interval for repeat exam. Primary variables include demographics, comorbidities, stage & location of cancer, and quality of bowel preparation. Secondary variables were the length of survival after diagnosis, morbidity and mortality of iCRC patients. Kaplan Meier analysis was used to assess survival. Binomial logistic regression analysis was used to assess risk factors and poor prognosis. Chi square analysis was used to assess comorbidities and type of CRC. P-value < 0.05 was considered statistically significant.
Results: 136 patients were diagnosed with CRC over a 10-year interval. Type of CRC, mean age, and statistical significance of comorbidities are listed in the table. Right-sided CRCs were significantly more common in the group with iCRC (p=0.01). Tumor location and iCRC versus non-iCRC were not associated with prognosis (p >0.05), but older age at diagnosis (OR = 1.07 [1.02-1.12]; p=0.005) and advanced stage of cancer (OR=2.60 [1.02-6.63]; p=0.045) were significantly associated with poor prognosis. Of the 27 iCRC patients, 13 died with iCRC cited as the reason for hospice in 7. Median survival time (yrs) of iCRC and non-iCRC patients were 3.20 (95% CI 1.47-4.92) and 6.20 (95% CI 3.29-9.10), respectively (NS).
Discussion: iCRCs comprised nearly 20% of total CRC cases in this series . The iCRC group tended to be older but there were no other clinical factors that differed between the iCRC and non-iCRC groups. The quality of bowel preparation documented on the prior colonoscopies of the iCRC group was adequate in most cases, making it unlikely that inadequate visualization was a major factor. The higher frequency of right-sided CRCs in iCRCs suggests that flat polyps that were missed may contribute to iCRCs.

Figure: Figure 1. Kaplan Meier Analysis of Survival Time Between iCRC and non-iCRC Patients
Disclosures:
Daniel Mai indicated no relevant financial relationships.
Estefania Flores indicated no relevant financial relationships.
Kyle Brown indicated no relevant financial relationships.
Daniel Mai, 1, Estefania Flores, MD2, Kyle Brown, MD2. P1776 - Retrospective Analysis of the Frequency, Risk Factors, and Clinical Outcomes of Interval Colorectal Cancer at a VA Medical Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
