Monday Poster Session
Category: Endoscopy Video Forum
P1801 - Curative Endoscopic Resection of a Gastric Inflammatory Myofibroblastic Tumor via Hybrid Endoscopic Submucosal Dissection
Alexander M. Carlson, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
1University at Buffalo, Buffalo, NY; 2Roswell Park Cancer Institute, Buffalo, NY; 3SUNY Upstate Medical University, Syracuse, NY
Introduction:
Inflammatory Myofibroblastic Tumor (IMT) is a rare intermediate neoplasm comprised of immune cells, smooth muscle and connective tissue. We report the case of an antral IMT that was removed via hybrid Endoscopic Submucosal Dissection. This resection was aided by the use of a through-the-scope helical tack suture device that permitted the efficient and durable closure of a large resection defect.
Case Description/Methods:
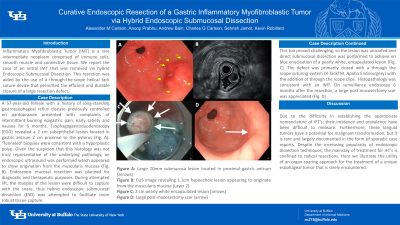
A 57-year-old female with a history of long-standing gastroesophageal reflux disease previously controlled on pantoprazole presented with complaints of intermittent burning epigastric pain, early satiety and nausea for 6 months. Esophagogastroduodenoscopy (EGD) revealed a 2 cm subepithelial lesion located in gastric antrum 2 cm proximal to the pylorus (Fig. A). ‘Tunneled’ biopsies were consistent with a hyperplastic polyp. Given the suspicion that this histology was not truly representative of the underlying pathology, an endoscopic ultrasound was performed which appeared to show origination from the muscularis mucosa (Fig. B). Endoscopic mucosal resection was planned for diagnostic and therapeutic purposes. During attempted lift, the margins of the lesion were difficult to capture with the snare, thus hybrid endoscopic submucosal dissection (ESD) was attempted to facilitate more robust tissue capture. This too proved challenging, so the lesion was unroofed and direct submucosal dissection was performed to achieve en bloc enucleation of a pearly white, encapsulated lesion (Fig. C). The defect was primarily closed with a through the scope suturing system (X-TackTM, Apollo Endosurgery) with the addition of through the scope clips. Histopathology was consistent with an IMT. On surveillance endoscopy 6 months after the resection, a large post mucosectomy scar was appreciated (Fig. D).
Discussion:
IMT’s of the gastrointestinal tract are uncommon, with the first description of a gastric IMT was by Soga et al. in 1970. The hallmark of an IMT is the dissociation between clinical presentation and histologic appearance. Clinically, the lesion appears malignant, but histology suggests a benign pathology. Despite the unclear risk of malignant transformation of IMT, complete surgical resection remains the standard of care. This case illustrates the safety and utility of an endoscopic, organ-sparing approach for a rare gastric tumor. When applicable, ESD offers a less invasive option with fewer complications when compared to surgical treatments for gastric IMT.

Figure B: EUS image revealing 1.1cm hypoechoic lesion appearing to originate from the muscularis mucosa (Layer 2)
Figure C: 2cm pearly white encapsulated lesion (arrows)
Figure D: Large post-mucosectomy scar (arrow)
Disclosures:
Alexander M. Carlson, DO1, Anoop Prabhu, MD2, Andrew Bain, MD2, Charles G. Carlson, BS3, Sehrish Jamot, MD2, Kevin Robillard, MD2. P1801 - Curative Endoscopic Resection of a Gastric Inflammatory Myofibroblastic Tumor via Hybrid Endoscopic Submucosal Dissection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
