Monday Poster Session
Category: Esophagus
P1806 - Potential Protective Effects of Eosinophilic Esophagitis in COVID-19 Infection: A Nearest Neighbor Propensity Score Matching Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Jennifer Hou, MD, PhD
Scripps Clinic/Scripps Green
La Jolla, CA
Presenting Author(s)
Jennifer Hou, MD, PhD1, Sang Hee K. Choi, MD2, Leah H.. Puglisi, MS3, Sam Mouwakeh, 4, Laura J.. Nicholson, MD, PhD5, Andrew A.. White, MD6, Quan M.. Nhu, MD, PhD7
1Scripps Clinic/Scripps Green, La Jolla, CA; 2Scripps Clinic/Scripps Green Hospital, La Jolla, CA; 3Scripps Whittier Diabetes Institute, San Diego, CA; 4Scripps Health, La Jolla, CA; 5Scripps Research Institute, La Jolla, CA; 6Scripps Clinic, La Jolla, CA; 7Scripps Clinic & Scripps Research Institute, La Jolla, CA
Introduction: The COVID-19 pandemic ignited global efforts, seeking to understand the mechanisms of SARS-CoV-2 pathogenesis and to identify protective factors. Patients with eosinophilic gastrointestinal disorders (EGID), i.e. eosinophilic esophagitis (EoE) have been reported to have similar to improved COVID-19 severity compared to non-EGID. Separately, low peripheral eosinophil levels correlate with worsened COVID-19. This study aims to investigate whether having EoE correlates with improved COVID-19 outcomes. Thus, this study seeks to offer insights into whether eosinophil recruitment and activation in EoE may be beneficial in COVID-19 survival.
Methods: This IRB-approved retrospective cohort study evaluated patients admitted with COVID-19 (12/2019-7/2022) to one of 5 campuses across our healthcare system, the largest in San Diego County. Outcomes included COVID-19 severity: all-cause mortality, acute hypoxemic respiratory failure, and ICU care. Given the disproportionate number of EoE vs. non-EoE, we applied a nearest neighbor propensity score matching, to identify cases most similar to those of interest for the control group. Patients were matched on baseline characteristics (Table 1).
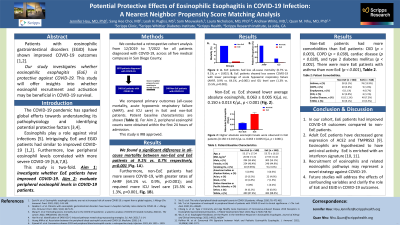
Results: Our study identified 5978 patients. We found a significant difference in all-cause mortality between non-EoE and EoE at 9.1% vs. 0.7% respectively, p< 0.001 (Fig. 1A). Non-EoE showed more severe COVID-19 than EoE with greater rates of acute hypoxemic respiratory failure (64.1% vs. 0.9%, p< 0.001); and more ICU care (15.5% vs. 1.3%, p< 0.001, Fig. 1B). Non-EoE vs. EoE showed lower average absolute eosinophils, 0.063±0.005K/μL vs. 0.150±0.013K/μL, p< 0.001 (Fig. 1C). Additional variables included current smoker wherein non-EoE had a significant difference vs. EoE (7.3% vs. 1.6%, p< 0.001). Non-EoE vs. EoE also had fewer patients with asthma (5.1% vs. 13.9%; p< 0.001) and more with CKD (4% vs. 1.1%; p=0.003), COPD (3.6% vs. 1.6%, p=0.038), cardiac disease (11.1% vs. 7.3%, p=0.028), type-2 diabetes mellitus (9.1% vs. 3.5%, p< 0.001).
Discussion: EoE compared to matched controls had significantly lower all-cause mortality and less severe COVID-19 disease. Our study highlights the potential protective role of type-2 immunity in COVID-19 for which eosinophils are a biomarker. Better understanding of the role of key cellular players and signaling pathways may lead to viable therapeutic targets. Future studies will further address the effects of confounding variables and clarify the role of EoE in COVID-19 outcomes.

Disclosures:
Jennifer Hou, MD, PhD1, Sang Hee K. Choi, MD2, Leah H.. Puglisi, MS3, Sam Mouwakeh, 4, Laura J.. Nicholson, MD, PhD5, Andrew A.. White, MD6, Quan M.. Nhu, MD, PhD7. P1806 - Potential Protective Effects of Eosinophilic Esophagitis in COVID-19 Infection: A Nearest Neighbor Propensity Score Matching Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Scripps Clinic/Scripps Green, La Jolla, CA; 2Scripps Clinic/Scripps Green Hospital, La Jolla, CA; 3Scripps Whittier Diabetes Institute, San Diego, CA; 4Scripps Health, La Jolla, CA; 5Scripps Research Institute, La Jolla, CA; 6Scripps Clinic, La Jolla, CA; 7Scripps Clinic & Scripps Research Institute, La Jolla, CA
Introduction: The COVID-19 pandemic ignited global efforts, seeking to understand the mechanisms of SARS-CoV-2 pathogenesis and to identify protective factors. Patients with eosinophilic gastrointestinal disorders (EGID), i.e. eosinophilic esophagitis (EoE) have been reported to have similar to improved COVID-19 severity compared to non-EGID. Separately, low peripheral eosinophil levels correlate with worsened COVID-19. This study aims to investigate whether having EoE correlates with improved COVID-19 outcomes. Thus, this study seeks to offer insights into whether eosinophil recruitment and activation in EoE may be beneficial in COVID-19 survival.
Methods: This IRB-approved retrospective cohort study evaluated patients admitted with COVID-19 (12/2019-7/2022) to one of 5 campuses across our healthcare system, the largest in San Diego County. Outcomes included COVID-19 severity: all-cause mortality, acute hypoxemic respiratory failure, and ICU care. Given the disproportionate number of EoE vs. non-EoE, we applied a nearest neighbor propensity score matching, to identify cases most similar to those of interest for the control group. Patients were matched on baseline characteristics (Table 1).
Results: Our study identified 5978 patients. We found a significant difference in all-cause mortality between non-EoE and EoE at 9.1% vs. 0.7% respectively, p< 0.001 (Fig. 1A). Non-EoE showed more severe COVID-19 than EoE with greater rates of acute hypoxemic respiratory failure (64.1% vs. 0.9%, p< 0.001); and more ICU care (15.5% vs. 1.3%, p< 0.001, Fig. 1B). Non-EoE vs. EoE showed lower average absolute eosinophils, 0.063±0.005K/μL vs. 0.150±0.013K/μL, p< 0.001 (Fig. 1C). Additional variables included current smoker wherein non-EoE had a significant difference vs. EoE (7.3% vs. 1.6%, p< 0.001). Non-EoE vs. EoE also had fewer patients with asthma (5.1% vs. 13.9%; p< 0.001) and more with CKD (4% vs. 1.1%; p=0.003), COPD (3.6% vs. 1.6%, p=0.038), cardiac disease (11.1% vs. 7.3%, p=0.028), type-2 diabetes mellitus (9.1% vs. 3.5%, p< 0.001).
Discussion: EoE compared to matched controls had significantly lower all-cause mortality and less severe COVID-19 disease. Our study highlights the potential protective role of type-2 immunity in COVID-19 for which eosinophils are a biomarker. Better understanding of the role of key cellular players and signaling pathways may lead to viable therapeutic targets. Future studies will further address the effects of confounding variables and clarify the role of EoE in COVID-19 outcomes.

Figure: Figure 1: A. EoE patients had less all-cause mortality. B. EoE patients demonstrated less severe COVID-19 disease course with lower percentage of acute hypoxemic respiratory failure (AHRF) and ICU level care. C. Higher absolute eosinophil levels were observed in EoE patients.
Disclosures:
Jennifer Hou indicated no relevant financial relationships.
Sang Hee Choi indicated no relevant financial relationships.
Leah Puglisi indicated no relevant financial relationships.
Sam Mouwakeh indicated no relevant financial relationships.
Laura Nicholson indicated no relevant financial relationships.
Andrew White: Amgen – Speakers Bureau. AstraZenca – Grant/Research Support, Speakers Bureau. Blueprint Pharmaceuticals – Advisory Committee/Board Member, Speakers Bureau. Cogent Pharmaceuticals – Advisory Committee/Board Member. GSK – Advisory Committee/Board Member, Speakers Bureau. Optinose – Advisory Committee/Board Member, Speakers Bureau. Regeneron/Sanofi – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau.
Quan Nhu: Regeneron – Advisory Committee/Board Member, Speakers Bureau. Sanofi – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member.
Jennifer Hou, MD, PhD1, Sang Hee K. Choi, MD2, Leah H.. Puglisi, MS3, Sam Mouwakeh, 4, Laura J.. Nicholson, MD, PhD5, Andrew A.. White, MD6, Quan M.. Nhu, MD, PhD7. P1806 - Potential Protective Effects of Eosinophilic Esophagitis in COVID-19 Infection: A Nearest Neighbor Propensity Score Matching Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

