Sunday Poster Session
Category: Biliary/Pancreas
P0013 - Outcomes for Cholangitis During the Covid-19 Pandemic and Comparison to 2019 from a Nationwide Database
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aizaz Khan, MD
University of Massachusetts Chan Medical School-Baystate
Springfield, Massachusetts
Presenting Author(s)
Aizaz Khan, MD1, Kamesh Gupta, MD2, Victoria Caruso, DO2
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2University of Massachusetts-Chan Baystate Medical Center, Springfield, MA
Introduction: During the Covid pandemic, many delays were reported in medical emergencies, both in time to presentation and the response time, leading to worse outcomes. Cholangitis carries high mortality rates and requires urgent resuscitation and endoscopy. To date, the impact of COVID-19 on cholangitis pathways and related outcomes in the United States remains unclear.
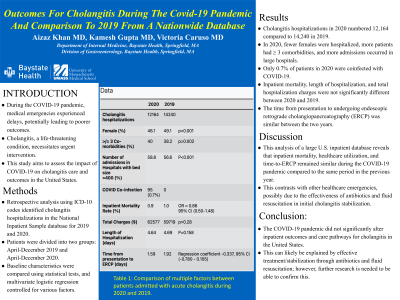
Methods: Using ICD-10 codes, we identified records for adult patients hospitalized for cholangitis from the National Inpatient Sample (NIS) database 2019 and 2020. We divided the patients into 2 groups: those admitted from April-December 2019 and those from April-December 2020. Baseline characteristics were compared using t-test and chi-square tests. Our data was analyzed using a multivariate logistic regression model to control for age, race, Charlson comorbidity index, intensive care unit (ICU) admission, shock, and acute renal failure.
Results: Cholangitis hospitalization numbered 12,164 in 2020 and 14,240 in 2019. In 2020, there were fewer females than in 2019 (46.1% vs 49.1%, p< 0.001), more patients had ≥ 3 comorbidities (40% vs 38.2%, p=0.002) and more number of admissions occurred in hospitals with bed size >400 (58.8% vs 56.6%, p< 0.001). 95 patients (0.7%) were coinfected with COVID-19 during 2020. There was no difference in the inpatient mortality rate between 2020 and 2019 (0.9% vs 1.0%, odds ratio 0.86, 95% confidence interval 0.50-1.48). Length of hospitalization (4.64 days vs 4.69 days, p=0.158) and total hospitalization charges ($62577 vs $59719, p=0.28) were not significantly different between 2020 and 2019. Total duration from presentation to undergoing endoscopic retrograde cholangiopancreatography (ERCP) was similar between 2020 and 2019 (1.59 days vs 1.92 days, regression coefficient -0.337, 95% CI -0.780 to 0.105).
Discussion: Analysis from the largest database for inpatient stays in the United States shows that the inpatient mortality rate and healthcare utilization were similar between the pandemic period (April-December 2020) to the same period for 2019. Time-to-ERCP was also similar. These findings differ from other healthcare emergencies such as variceal bleeding or acute coronary syndrome. One possible explanation for this difference is that antibiotics are effective at initial stabilization for cholangitis unlike others which require urgent invasive procedures. Baseline characteristics were largely similar between the 2 groups indicating a representative population with less chances of selection bias.
Disclosures:
Aizaz Khan, MD1, Kamesh Gupta, MD2, Victoria Caruso, DO2. P0013 - Outcomes for Cholangitis During the Covid-19 Pandemic and Comparison to 2019 from a Nationwide Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2University of Massachusetts-Chan Baystate Medical Center, Springfield, MA
Introduction: During the Covid pandemic, many delays were reported in medical emergencies, both in time to presentation and the response time, leading to worse outcomes. Cholangitis carries high mortality rates and requires urgent resuscitation and endoscopy. To date, the impact of COVID-19 on cholangitis pathways and related outcomes in the United States remains unclear.
Methods: Using ICD-10 codes, we identified records for adult patients hospitalized for cholangitis from the National Inpatient Sample (NIS) database 2019 and 2020. We divided the patients into 2 groups: those admitted from April-December 2019 and those from April-December 2020. Baseline characteristics were compared using t-test and chi-square tests. Our data was analyzed using a multivariate logistic regression model to control for age, race, Charlson comorbidity index, intensive care unit (ICU) admission, shock, and acute renal failure.
Results: Cholangitis hospitalization numbered 12,164 in 2020 and 14,240 in 2019. In 2020, there were fewer females than in 2019 (46.1% vs 49.1%, p< 0.001), more patients had ≥ 3 comorbidities (40% vs 38.2%, p=0.002) and more number of admissions occurred in hospitals with bed size >400 (58.8% vs 56.6%, p< 0.001). 95 patients (0.7%) were coinfected with COVID-19 during 2020. There was no difference in the inpatient mortality rate between 2020 and 2019 (0.9% vs 1.0%, odds ratio 0.86, 95% confidence interval 0.50-1.48). Length of hospitalization (4.64 days vs 4.69 days, p=0.158) and total hospitalization charges ($62577 vs $59719, p=0.28) were not significantly different between 2020 and 2019. Total duration from presentation to undergoing endoscopic retrograde cholangiopancreatography (ERCP) was similar between 2020 and 2019 (1.59 days vs 1.92 days, regression coefficient -0.337, 95% CI -0.780 to 0.105).
Discussion: Analysis from the largest database for inpatient stays in the United States shows that the inpatient mortality rate and healthcare utilization were similar between the pandemic period (April-December 2020) to the same period for 2019. Time-to-ERCP was also similar. These findings differ from other healthcare emergencies such as variceal bleeding or acute coronary syndrome. One possible explanation for this difference is that antibiotics are effective at initial stabilization for cholangitis unlike others which require urgent invasive procedures. Baseline characteristics were largely similar between the 2 groups indicating a representative population with less chances of selection bias.
Disclosures:
Aizaz Khan indicated no relevant financial relationships.
Kamesh Gupta indicated no relevant financial relationships.
Victoria Caruso indicated no relevant financial relationships.
Aizaz Khan, MD1, Kamesh Gupta, MD2, Victoria Caruso, DO2. P0013 - Outcomes for Cholangitis During the Covid-19 Pandemic and Comparison to 2019 from a Nationwide Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

