Sunday Poster Session
Category: Biliary/Pancreas
P0092 - Lemmel Syndrome: A Rare Cause of Obstructive Jaundice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Jiteshwar S. Pannu, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Jiteshwar S. Pannu, MD1, Michael Sutton, MD2, John Maple, DO1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Lemmel syndrome (LS) is a rare phenomenon manifesting as obstructive jaundice due to biliary compression by a periampullary duodenal diverticula (PDD), in the absence of other obstructing pathology. Due to its infrequent occurrence, it may be overlooked, yet can potentially lead to significant clinical morbidity. Herein, we present a patient diagnosed with obstructive jaundice due to periampullary diverticulitis i.e. LS, that was treated endoscopically.
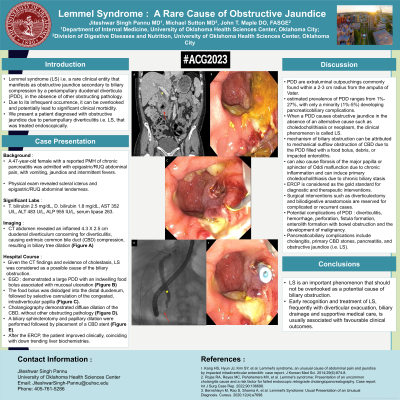
Case Description/Methods: A 47-year-old female was admitted with epigastric abdominal pain, vomiting, jaundice and intermittent fevers. Physical exam revealed scleral icterus and epigastric tenderness. Pertinent labs included T. bilirubin 2.5 mg/dL, D. bilirubin 1.8 mg/dL, AST 352 U/L, ALT 483 U/L, ALP 955 IU/L, serum lipase 263. CT abdomen revealed a 4.3 X 2.5 cm inflamed duodenal diverticulum, causing extrinsic common bile duct (CBD) compression and biliary tree dilation. Given the CT findings and evidence of cholestasis, LS was considered as a possible cause of biliary obstruction. Patient subsequently underwent an ERCP that demonstrated a large PDD with an indwelling food bolus associated with mucosal ulceration. The food bolus was dislodged into the distal duodenum, followed by selective cannulation of the congested, intradiverticular papilla. Cholangiography demonstrated diffuse dilation of the CBD, without other obstructing pathology. A biliary sphincterotomy and papillary dilation were performed followed by placement of a CBD stent. After the ERCP, the patient improved clinically, coinciding with down trending liver biochemistries.
Discussion: The estimated prevalence of PDD ranges from 1%-27%, with only a minority (1%-5%) developing pancreaticobiliary complications. The mechanism of developing LS can be attributed to mechanical outflow obstruction due to the debris/enterolith filled PDD, fibrosis of the major papilla with sphincter of Oddi malfunction due to chronic inflammation or induction of primary choledocholithiasis from chronic biliary stasis and bacterial overgrowth. While diagnosis is aided by imaging modalities such as CT or MRCP, ERCP is considered as the gold standard for diagnostic and therapeutic interventions. Surgical interventions such as diverticulectomy and biliodigestive anastomosis are reserved for complicated or recurrent cases. Early recognition and treatment of LS, frequently with diverticular evacuation, biliary drainage and supportive medical care, is usually associated with favorable clinical outcomes.

Disclosures:
Jiteshwar S. Pannu, MD1, Michael Sutton, MD2, John Maple, DO1. P0092 - Lemmel Syndrome: A Rare Cause of Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK
Introduction: Lemmel syndrome (LS) is a rare phenomenon manifesting as obstructive jaundice due to biliary compression by a periampullary duodenal diverticula (PDD), in the absence of other obstructing pathology. Due to its infrequent occurrence, it may be overlooked, yet can potentially lead to significant clinical morbidity. Herein, we present a patient diagnosed with obstructive jaundice due to periampullary diverticulitis i.e. LS, that was treated endoscopically.
Case Description/Methods: A 47-year-old female was admitted with epigastric abdominal pain, vomiting, jaundice and intermittent fevers. Physical exam revealed scleral icterus and epigastric tenderness. Pertinent labs included T. bilirubin 2.5 mg/dL, D. bilirubin 1.8 mg/dL, AST 352 U/L, ALT 483 U/L, ALP 955 IU/L, serum lipase 263. CT abdomen revealed a 4.3 X 2.5 cm inflamed duodenal diverticulum, causing extrinsic common bile duct (CBD) compression and biliary tree dilation. Given the CT findings and evidence of cholestasis, LS was considered as a possible cause of biliary obstruction. Patient subsequently underwent an ERCP that demonstrated a large PDD with an indwelling food bolus associated with mucosal ulceration. The food bolus was dislodged into the distal duodenum, followed by selective cannulation of the congested, intradiverticular papilla. Cholangiography demonstrated diffuse dilation of the CBD, without other obstructing pathology. A biliary sphincterotomy and papillary dilation were performed followed by placement of a CBD stent. After the ERCP, the patient improved clinically, coinciding with down trending liver biochemistries.
Discussion: The estimated prevalence of PDD ranges from 1%-27%, with only a minority (1%-5%) developing pancreaticobiliary complications. The mechanism of developing LS can be attributed to mechanical outflow obstruction due to the debris/enterolith filled PDD, fibrosis of the major papilla with sphincter of Oddi malfunction due to chronic inflammation or induction of primary choledocholithiasis from chronic biliary stasis and bacterial overgrowth. While diagnosis is aided by imaging modalities such as CT or MRCP, ERCP is considered as the gold standard for diagnostic and therapeutic interventions. Surgical interventions such as diverticulectomy and biliodigestive anastomosis are reserved for complicated or recurrent cases. Early recognition and treatment of LS, frequently with diverticular evacuation, biliary drainage and supportive medical care, is usually associated with favorable clinical outcomes.

Figure: Figure A : CT of the abdomen showing a 4.3 X 2.5 cm duodenal diverticulum with surrounding inflammation (red arrow) concerning for diverticulitis, causing common bile duct compression via mass effect, resulting in biliary tree dilation (yellow star); Figure B : EGD showing a large peri-ampullary duodenal diverticulum with an indwelling food bolus associated with extensive mucosal ulceration; Figure C : Selective cannulation of the congested, intradiverticular papilla; Figure D : Cholangiography revealing diffuse dilation of the CBD (yellow star), with evidence of obstruction in the peri-ampullary region (red arrow); Figure E : Papillary dilation and placement of a CBD stent through the congested, intradiverticular papilla
Disclosures:
Jiteshwar Pannu indicated no relevant financial relationships.
Michael Sutton indicated no relevant financial relationships.
John Maple indicated no relevant financial relationships.
Jiteshwar S. Pannu, MD1, Michael Sutton, MD2, John Maple, DO1. P0092 - Lemmel Syndrome: A Rare Cause of Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
