Sunday Poster Session
Category: Biliary/Pancreas
P0119 - Symptomatic Anemia Following Acute Pancreatitis: An Unusual Cause
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Alaa Taha, MD
Wayne State University/Ascension Providence Rochester Hospital
Rochester, MI
Presenting Author(s)
Alaa Taha, MD1, Tripti Nagar, MD2, Wadid Sirri, MD1, Vesna Tegeltija, MD3, Zachary Johnson, MD4
1Wayne State University/Ascension Providence Rochester Hospital, Rochester, MI; 2Wayne State University, Detroit, MI; 3Wayne State University GME, Rochester, MI; 4Ascension Providence Rochester Hospital, Rochester, MI
Introduction: Acute pancreatitis is a leading cause of inpatient admissions for gastrointestinal disorders. It has many complications which can be systemic and local. Splanchnic vein thrombosis is one complication that is usually seen in severe acute pancreatitis. When it involves the splenic vein, it can lead to splenic rupture. The proposed mechanism is venous outflow obstruction leading to gradual congestion within the splenic parenchyma. We present a case of a 42-year-old male who had significant anemia secondary to splenic rupture one week after being hospitalized for acute necrotizing pancreatitis.
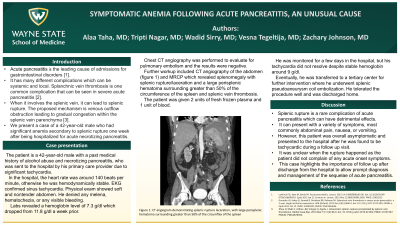
Case Description/Methods: The patient is a 42-year-old male with a past medical history of alcohol abuse and necrotizing pancreatitis who was sent to the hospital by his primary care provider due to significant tachycardia. In the hospital, the heart rate was around 140 beats per minute, otherwise, he was hemodynamically stable. EKG confirmed sinus tachycardia. Labs revealed a hemoglobin level of 7.3 g/dl which dropped from 11.8 g/dl a week prior. He denied melena, hematochezia, or any visible bleeding. Chest CT angiography was performed to evaluate for pulmonary embolism and the results were negative. Further workup included CT angiography of the abdomen and MRCP which revealed splenomegaly with splenic rupture/laceration and a large perisplenic hematoma surrounding greater than 50% of the circumference of the spleen and splenic vein thrombosis. He was given 2 units of fresh frozen plasma and 1 unit of blood. He was monitored for a few days in the hospital, but his tachycardia did not resolve despite the hemoglobin being stable around 9 g/dl. Eventually, he was transferred to a tertiary center where he underwent splenic pseudoaneurysm coil embolization. He tolerated the procedure well and was discharged home.
Discussion: Splenic rupture is a rare complication of acute pancreatitis which can have detrimental effects. It can present with a variety of symptoms, most commonly abdominal pain, nausea, or vomiting. However, this patient was overall asymptomatic and presented to the hospital after he was found to be tachycardic during a follow up visit. It was unclear when the rupture happened as the patient did not complain of any acute onset symptoms. This case highlights the importance of follow up after discharge from the hospital to allow prompt diagnosis and management of the sequelae of acute pancreatitis.

Disclosures:
Alaa Taha, MD1, Tripti Nagar, MD2, Wadid Sirri, MD1, Vesna Tegeltija, MD3, Zachary Johnson, MD4. P0119 - Symptomatic Anemia Following Acute Pancreatitis: An Unusual Cause, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University/Ascension Providence Rochester Hospital, Rochester, MI; 2Wayne State University, Detroit, MI; 3Wayne State University GME, Rochester, MI; 4Ascension Providence Rochester Hospital, Rochester, MI
Introduction: Acute pancreatitis is a leading cause of inpatient admissions for gastrointestinal disorders. It has many complications which can be systemic and local. Splanchnic vein thrombosis is one complication that is usually seen in severe acute pancreatitis. When it involves the splenic vein, it can lead to splenic rupture. The proposed mechanism is venous outflow obstruction leading to gradual congestion within the splenic parenchyma. We present a case of a 42-year-old male who had significant anemia secondary to splenic rupture one week after being hospitalized for acute necrotizing pancreatitis.
Case Description/Methods: The patient is a 42-year-old male with a past medical history of alcohol abuse and necrotizing pancreatitis who was sent to the hospital by his primary care provider due to significant tachycardia. In the hospital, the heart rate was around 140 beats per minute, otherwise, he was hemodynamically stable. EKG confirmed sinus tachycardia. Labs revealed a hemoglobin level of 7.3 g/dl which dropped from 11.8 g/dl a week prior. He denied melena, hematochezia, or any visible bleeding. Chest CT angiography was performed to evaluate for pulmonary embolism and the results were negative. Further workup included CT angiography of the abdomen and MRCP which revealed splenomegaly with splenic rupture/laceration and a large perisplenic hematoma surrounding greater than 50% of the circumference of the spleen and splenic vein thrombosis. He was given 2 units of fresh frozen plasma and 1 unit of blood. He was monitored for a few days in the hospital, but his tachycardia did not resolve despite the hemoglobin being stable around 9 g/dl. Eventually, he was transferred to a tertiary center where he underwent splenic pseudoaneurysm coil embolization. He tolerated the procedure well and was discharged home.
Discussion: Splenic rupture is a rare complication of acute pancreatitis which can have detrimental effects. It can present with a variety of symptoms, most commonly abdominal pain, nausea, or vomiting. However, this patient was overall asymptomatic and presented to the hospital after he was found to be tachycardic during a follow up visit. It was unclear when the rupture happened as the patient did not complain of any acute onset symptoms. This case highlights the importance of follow up after discharge from the hospital to allow prompt diagnosis and management of the sequelae of acute pancreatitis.

Figure: CT angiogram of the abdomen showing splenic rupture/laceration with large perisplenic hematoma
Disclosures:
Alaa Taha indicated no relevant financial relationships.
Tripti Nagar indicated no relevant financial relationships.
Wadid Sirri indicated no relevant financial relationships.
Vesna Tegeltija indicated no relevant financial relationships.
Zachary Johnson indicated no relevant financial relationships.
Alaa Taha, MD1, Tripti Nagar, MD2, Wadid Sirri, MD1, Vesna Tegeltija, MD3, Zachary Johnson, MD4. P0119 - Symptomatic Anemia Following Acute Pancreatitis: An Unusual Cause, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
