Sunday Poster Session
Category: Biliary/Pancreas
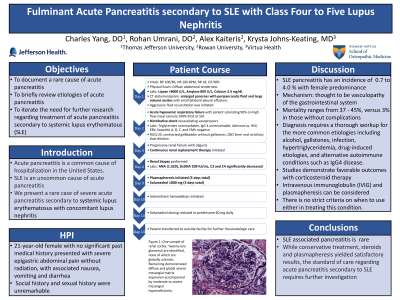
P0125 - Fulminant Acute Pancreatitis Secondary to SLE with Class Four to Five Lupus Nephritis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Charles Yang, DO
Thomas Jefferson University
Voorhees, NJ
Presenting Author(s)
Charles Yang, DO1, Rohan Umrani, DO2, Andy Mai, DO1, Elizabeth Ko, DO1, Alex Kaiteris, 2, Krysta Johns-Keating, MD3
1Thomas Jefferson University, Voorhees, NJ; 2Rowan University, Voorhees, NJ; 3Virtua Health, Camden, NJ
Introduction: Acute pancreatitis is a common cause of hospitalization in the United States. Systemic lupus erythematosus (SLE) is an uncommon cause of acute pancreatitis. We present a rare case of severe acute pancreatitis secondary to systemic lupus erythematosus with concomitant lupus nephritis.
Case Description/Methods: A 21-year-old female with no significant past medical history presented with severe epigastric abdominal pain with associated nausea and vomiting. She denied drug use, alcohol use, recent travel and new medications. Vitals were significant for blood pressure of 110/86, heart rate 100bpm, respiratory rate 18, oxygen saturation 98% on room air. Unfortunately, the patient rapidly deteriorated, requiring high flow nasal cannula and vasopressors. Physical exam was notable for diffuse abdominal tenderness without rash. Labs were significant for lipase >8000 U/L, amylase 809 U/L. Triglycerides and IgG4 within normal limits. Infectious panels were negative. Computed tomography of the abdomen and pelvis demonstrated an enlarged pancreas with peripancreatic fluid. Ultrasound of the right upper quadrant demonstrated no gallstones nor biliary duct dilatation. Magnetic resonance cholangiopancreatography demonstrated diffuse edema of the pancreas with no ductal abnormalities. Autoimmune panel was positive for ANA (1:320), double stranded DNA 209 IU/mL, with decreased C3 and C4. Renal biopsy demonstrated class four to five lupus nephritis. The patient underwent plasmapheresis for five sessions, supplemented with methylprednisolone 1,000 mg for three doses. By day 14, she was transferred for further rheumatologic management.
Discussion: Lupus associated pancreatitis has an incidence of 0.7 to 4.0 percent with higher prevalence in females in the third decade of life. While the exact etiology is unknown, vasculopathy of the gastrointestinal system is one of the most commonly proposed mechanisms. Mortality appears to be highly linked to the incidence of concurrent complications. Diagnosis of SLE pancreatitis requires a thorough workup for the more common etiologies including alcohol, gallstones, infection, triglycerides, and autoimmune conditions. In most studies, patients treated with high dose corticosteroids had favorable outcomes. Intravenous immunoglobulin and plasmapheresis are additional options in severe cases. There is no strict criteria on when to use either in treating this condition. Further research is needed to understand the utility of these modalities in treatment of SLE pancreatitis.

Disclosures:
Charles Yang, DO1, Rohan Umrani, DO2, Andy Mai, DO1, Elizabeth Ko, DO1, Alex Kaiteris, 2, Krysta Johns-Keating, MD3. P0125 - Fulminant Acute Pancreatitis Secondary to SLE with Class Four to Five Lupus Nephritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Thomas Jefferson University, Voorhees, NJ; 2Rowan University, Voorhees, NJ; 3Virtua Health, Camden, NJ
Introduction: Acute pancreatitis is a common cause of hospitalization in the United States. Systemic lupus erythematosus (SLE) is an uncommon cause of acute pancreatitis. We present a rare case of severe acute pancreatitis secondary to systemic lupus erythematosus with concomitant lupus nephritis.
Case Description/Methods: A 21-year-old female with no significant past medical history presented with severe epigastric abdominal pain with associated nausea and vomiting. She denied drug use, alcohol use, recent travel and new medications. Vitals were significant for blood pressure of 110/86, heart rate 100bpm, respiratory rate 18, oxygen saturation 98% on room air. Unfortunately, the patient rapidly deteriorated, requiring high flow nasal cannula and vasopressors. Physical exam was notable for diffuse abdominal tenderness without rash. Labs were significant for lipase >8000 U/L, amylase 809 U/L. Triglycerides and IgG4 within normal limits. Infectious panels were negative. Computed tomography of the abdomen and pelvis demonstrated an enlarged pancreas with peripancreatic fluid. Ultrasound of the right upper quadrant demonstrated no gallstones nor biliary duct dilatation. Magnetic resonance cholangiopancreatography demonstrated diffuse edema of the pancreas with no ductal abnormalities. Autoimmune panel was positive for ANA (1:320), double stranded DNA 209 IU/mL, with decreased C3 and C4. Renal biopsy demonstrated class four to five lupus nephritis. The patient underwent plasmapheresis for five sessions, supplemented with methylprednisolone 1,000 mg for three doses. By day 14, she was transferred for further rheumatologic management.
Discussion: Lupus associated pancreatitis has an incidence of 0.7 to 4.0 percent with higher prevalence in females in the third decade of life. While the exact etiology is unknown, vasculopathy of the gastrointestinal system is one of the most commonly proposed mechanisms. Mortality appears to be highly linked to the incidence of concurrent complications. Diagnosis of SLE pancreatitis requires a thorough workup for the more common etiologies including alcohol, gallstones, infection, triglycerides, and autoimmune conditions. In most studies, patients treated with high dose corticosteroids had favorable outcomes. Intravenous immunoglobulin and plasmapheresis are additional options in severe cases. There is no strict criteria on when to use either in treating this condition. Further research is needed to understand the utility of these modalities in treatment of SLE pancreatitis.

Figure: Figure 1: One sample of renal cortex. Twenty-one glomeruli are identified, none of which are globally sclerotic. Remaining demonstrated diffuse and global severe mesangial matrix expansion accompanied by moderate to severe mesangial hypercellularity.
Disclosures:
Charles Yang indicated no relevant financial relationships.
Rohan Umrani indicated no relevant financial relationships.
Andy Mai indicated no relevant financial relationships.
Elizabeth Ko indicated no relevant financial relationships.
Alex Kaiteris indicated no relevant financial relationships.
Krysta Johns-Keating indicated no relevant financial relationships.
Charles Yang, DO1, Rohan Umrani, DO2, Andy Mai, DO1, Elizabeth Ko, DO1, Alex Kaiteris, 2, Krysta Johns-Keating, MD3. P0125 - Fulminant Acute Pancreatitis Secondary to SLE with Class Four to Five Lupus Nephritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
