Sunday Poster Session
Category: Biliary/Pancreas
P0151 - Pseudocyst True Morbidity: Endoscopic Management of a Giant Pancreatic Pseudocyst
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Nathan E. Usry, MD
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Nathan E. Usry, MD, Anna Owings, DO, Parth Maheshwari, MD, Ismail Ganim, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Pancreatic pseudocysts are loculations of pancreatic fluid surrounded in a non-epithelialized capsule, thus rendering the name “pseudo” cysts as opposed to true cysts from a continuous epithelium. Usual formation is after a breakage in the pancreatic ductal system causing extravasation of enzymatic fluid due to inflammation or direct trauma. Incidence in chronic pancreatitis ranges from 20-40% as opposed to 5-16% of acute pancreatitis cases.
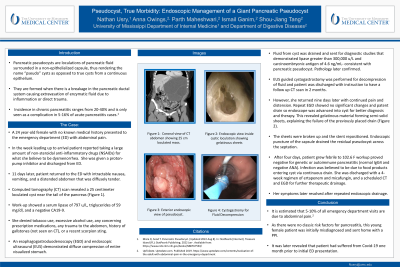
Case Description/Methods: A 24-year-old female with no known medical history presented to the ED with abdominal pain. She reported taking a large amount of NSAIDs for what she believed to be dysmenorrhea. She was given a PPI and discharged. 11 days later, she returned to ED with a distended abdomen and diffuse abdominal pain. CT scan revealed a 25 cm loculated cyst near tail of pancreas. Work-up revealed serum lipase of 797 U/L, triglycerides 59 mg/dl, and a negative CA19-9. She denied tobacco use or significant alcohol use. An EGD and endoscopic ultrasound (EUS) demonstrated diffuse compression of entire visualized stomach. Fluid from cyst was drained and sent for diagnostic studies that demonstrated lipase greater than 300,000 u/L and CEA of 4.6 ng/mL- consistent with pancreatic pseudocyst. Pathology later confirmed.
Cystogastrostomy tube was placed for decompression of fluid and patient was discharged with instruction to have a follow up CT scan in 2 months. However, she returned nine days later with continued pain and distension. Repeat EGD showed no significant changes and patent drain. The endoscope was advanced into cyst for better diagnosis and therapy. This revealed gelatinous material forming semi-solid sheets, explaining the failure of the previously placed drain. The sheets were broken up and the stent repositioned. After four days, patient grew febrile to 102.6 F. Further workup proved negative for genetic or autoimmune pancreatitis (normal IgG4 and negative ANA). Infection was believed to be due to food products entering cyst via continuous drain. She was discharged with a 4-week regimen of antimicrobials and a scheduled CT and EGD.
Discussion: It is estimated that 5-10% of all emergency department visits are due to abdominal pain. For this patient it was not until after obtaining imaging that the true pathology was identified. Though there is still no clear indication as to why this patient suffered from chronic pancreatitis and subsequent pseudocyst this case highlights the importance of abdominal pain differential diagnoses in young women.

Disclosures:
Nathan E. Usry, MD, Anna Owings, DO, Parth Maheshwari, MD, Ismail Ganim, MD. P0151 - Pseudocyst True Morbidity: Endoscopic Management of a Giant Pancreatic Pseudocyst, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Pancreatic pseudocysts are loculations of pancreatic fluid surrounded in a non-epithelialized capsule, thus rendering the name “pseudo” cysts as opposed to true cysts from a continuous epithelium. Usual formation is after a breakage in the pancreatic ductal system causing extravasation of enzymatic fluid due to inflammation or direct trauma. Incidence in chronic pancreatitis ranges from 20-40% as opposed to 5-16% of acute pancreatitis cases.
Case Description/Methods: A 24-year-old female with no known medical history presented to the ED with abdominal pain. She reported taking a large amount of NSAIDs for what she believed to be dysmenorrhea. She was given a PPI and discharged. 11 days later, she returned to ED with a distended abdomen and diffuse abdominal pain. CT scan revealed a 25 cm loculated cyst near tail of pancreas. Work-up revealed serum lipase of 797 U/L, triglycerides 59 mg/dl, and a negative CA19-9. She denied tobacco use or significant alcohol use. An EGD and endoscopic ultrasound (EUS) demonstrated diffuse compression of entire visualized stomach. Fluid from cyst was drained and sent for diagnostic studies that demonstrated lipase greater than 300,000 u/L and CEA of 4.6 ng/mL- consistent with pancreatic pseudocyst. Pathology later confirmed.
Cystogastrostomy tube was placed for decompression of fluid and patient was discharged with instruction to have a follow up CT scan in 2 months. However, she returned nine days later with continued pain and distension. Repeat EGD showed no significant changes and patent drain. The endoscope was advanced into cyst for better diagnosis and therapy. This revealed gelatinous material forming semi-solid sheets, explaining the failure of the previously placed drain. The sheets were broken up and the stent repositioned. After four days, patient grew febrile to 102.6 F. Further workup proved negative for genetic or autoimmune pancreatitis (normal IgG4 and negative ANA). Infection was believed to be due to food products entering cyst via continuous drain. She was discharged with a 4-week regimen of antimicrobials and a scheduled CT and EGD.
Discussion: It is estimated that 5-10% of all emergency department visits are due to abdominal pain. For this patient it was not until after obtaining imaging that the true pathology was identified. Though there is still no clear indication as to why this patient suffered from chronic pancreatitis and subsequent pseudocyst this case highlights the importance of abdominal pain differential diagnoses in young women.

Figure: Coronal view of CT abdomen with 25 cm pseudocyst.
Disclosures:
Nathan Usry indicated no relevant financial relationships.
Anna Owings indicated no relevant financial relationships.
Parth Maheshwari indicated no relevant financial relationships.
Ismail Ganim indicated no relevant financial relationships.
Nathan E. Usry, MD, Anna Owings, DO, Parth Maheshwari, MD, Ismail Ganim, MD. P0151 - Pseudocyst True Morbidity: Endoscopic Management of a Giant Pancreatic Pseudocyst, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
