Sunday Poster Session
Category: Biliary/Pancreas
P0157 - Estrogen-Induced Pancreatitis in a Transgender Female
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ushan A. Ranasinghe, MD, MS
Swedish Hospital, part of Northshore University Health System
Chicago, IL
Presenting Author(s)
Ushan A. Ranasinghe, MD, MS1, Regine Lim, BS2, Lukasz J. Jaros, MD3
1Swedish Hospital, part of Northshore University Health System, Chicago, IL; 2Midwestern University Chicago College of Osteopathic Medicine, Downers Grove, IL; 3Northwestern University, Chicago, IL
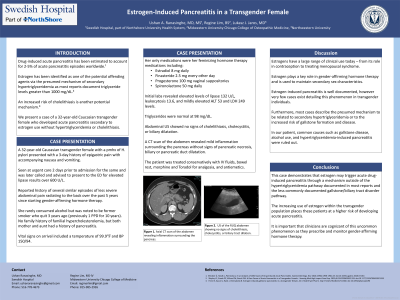
Introduction: Drug-induced acute pancreatitis has been estimated to account for 2-5% of acute pancreatitis episodes worldwide.1Estrogen has been identified as one of the potential offending agents via the mechanism of secondary hypertriglyceridemia as most reports document triglyceride levels greater than 1000 mg/dL.6 However, estrogen-induced pancreatitis is not well described in the transgender female population, with even fewer reports of acute pancreatitis related to estrogen use without hypertriglyceridemia. This case report documents a rare case of a 32-year-old Caucasian transgender female who developed acute pancreatitis secondary to estrogen use without hypertriglyceridemia.
Case Description/Methods: The patient presented to the emergency department with a three-day history of epigastric pain with accompanying nausea and vomiting. She was first seen at urgent care two days prior and was later advised to present to the ER for further evaluation of suspected pancreatitis due to an elevated lipase of over 600U/L. In the ED, the patient recalled over a dozen similar episodes of less severe abdominal pain radiating to the back intermittently over the past five years after starting Estrogen therapy. Blood tests revealed elevated levels of lipase (132 U/L), WBC (13.64x10³/uL), and mildly elevated ALT (53) and LDH (249). Serum blood urea nitrogen, creatinine, alkaline phosphatase, aspartate aminotransferase, bilirubin, and triglycerides (98) were within respective reference ranges. The patient also denied any alcohol use. An abdominal CT showed mild inflammation surrounding the pancreas without signs of pancreatic duct dilatation, necrosis, or biliary dilatation. A right upper quadrant ultrasound showed no signs of cholelithiasis or cholecystitis. The patient recovered with supportive therapy including intravenous hydration and analgesics. Her estradiol was discontinued during her admission.
Discussion: Estrogen is a key component of gender-affirming hormone therapy. Systemic estrogens have been identified as precipitators of acute pancreatitis. This case demonstrates that estrogen can trigger acute pancreatitis via a mechanism outside of the hypertriglyceridemia pathway documented in most reports. The use of this medication in the transgender community places these patients at a higher risk of developing acute pancreatitis. It is important that clinicians are cognizant of this uncommon phenomenon as they prescribe gender-affirming hormone therapy.
Disclosures:
Ushan A. Ranasinghe, MD, MS1, Regine Lim, BS2, Lukasz J. Jaros, MD3. P0157 - Estrogen-Induced Pancreatitis in a Transgender Female, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Swedish Hospital, part of Northshore University Health System, Chicago, IL; 2Midwestern University Chicago College of Osteopathic Medicine, Downers Grove, IL; 3Northwestern University, Chicago, IL
Introduction: Drug-induced acute pancreatitis has been estimated to account for 2-5% of acute pancreatitis episodes worldwide.1Estrogen has been identified as one of the potential offending agents via the mechanism of secondary hypertriglyceridemia as most reports document triglyceride levels greater than 1000 mg/dL.6 However, estrogen-induced pancreatitis is not well described in the transgender female population, with even fewer reports of acute pancreatitis related to estrogen use without hypertriglyceridemia. This case report documents a rare case of a 32-year-old Caucasian transgender female who developed acute pancreatitis secondary to estrogen use without hypertriglyceridemia.
Case Description/Methods: The patient presented to the emergency department with a three-day history of epigastric pain with accompanying nausea and vomiting. She was first seen at urgent care two days prior and was later advised to present to the ER for further evaluation of suspected pancreatitis due to an elevated lipase of over 600U/L. In the ED, the patient recalled over a dozen similar episodes of less severe abdominal pain radiating to the back intermittently over the past five years after starting Estrogen therapy. Blood tests revealed elevated levels of lipase (132 U/L), WBC (13.64x10³/uL), and mildly elevated ALT (53) and LDH (249). Serum blood urea nitrogen, creatinine, alkaline phosphatase, aspartate aminotransferase, bilirubin, and triglycerides (98) were within respective reference ranges. The patient also denied any alcohol use. An abdominal CT showed mild inflammation surrounding the pancreas without signs of pancreatic duct dilatation, necrosis, or biliary dilatation. A right upper quadrant ultrasound showed no signs of cholelithiasis or cholecystitis. The patient recovered with supportive therapy including intravenous hydration and analgesics. Her estradiol was discontinued during her admission.
Discussion: Estrogen is a key component of gender-affirming hormone therapy. Systemic estrogens have been identified as precipitators of acute pancreatitis. This case demonstrates that estrogen can trigger acute pancreatitis via a mechanism outside of the hypertriglyceridemia pathway documented in most reports. The use of this medication in the transgender community places these patients at a higher risk of developing acute pancreatitis. It is important that clinicians are cognizant of this uncommon phenomenon as they prescribe gender-affirming hormone therapy.
Disclosures:
Ushan Ranasinghe indicated no relevant financial relationships.
Regine Lim indicated no relevant financial relationships.
Lukasz Jaros indicated no relevant financial relationships.
Ushan A. Ranasinghe, MD, MS1, Regine Lim, BS2, Lukasz J. Jaros, MD3. P0157 - Estrogen-Induced Pancreatitis in a Transgender Female, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
