Sunday Poster Session
Category: Colon
P0215 - A Rare Case of Metastatic Melanoma to Cecum Found on Screening Colonoscopy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Rachael Schneider, DO
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Rachael Schneider, DO, Stefanie Gallagher, DO, Amanda Long, DO, Marc Zitin, MD
Lankenau Medical Center, Wynnewood, PA
Introduction: Metastatic melanoma is the fifth most common cause of cancer in the United States. The 5-year survival of metastatic melanoma is about 25%. The most common sites of metastasis are skin, lungs, liver, and bone. Metastasis to the gastrointestinal (GI) tract accounts for just 1-3% of malignant melanomas with the small intestine and stomach being the most common sites. We present the case of a patient with stage IV melanoma found to have colonic metastasis on screening colonoscopy.
Case Description/Methods: Patient is a 76-year-old male with a history of hypertension, diabetes, coronary artery disease, and melanoma in situ of his right parietal scalp and left arm diagnosed in 2014. The melanomas were excised, and he received pembrolizumab from 2015 to 2016. He underwent radical resection for metastasis to the left upper back in 2019 and 2021. He underwent routine PET and CT scans for surveillance. CT in January 2023 noted no new lesions. His last screening colonoscopy was 12 years prior and recent hemoglobin was normal and he was without any GI complaints. He underwent screening colonoscopy in April 2023 showing a large cecal fungating and ulcerated mass involving half of the lumen circumference. Pathology confirmed metastatic melanoma of the colon. Stains positive for HMB-45, Melan A, Sox10. PET scan showed an FDG avid cecal mass with adjacent metastatic mesenteric nodes. He was seen by colorectal surgery and oncology. Given his lack of symptoms, decision made to hold off on surgery and start immunotherapy alone.
Discussion: Colonic metastases account for 15.5% of melanoma metastasis to the GI tract and 0.3% of melanoma metastasis overall. This rarity is due to the absence of melanocytes in the colon. Most cases of metastasis to the colon are diagnosed post-mortem as most patients are asymptomatic. The most common symptom is GI bleeding. Metastatic melanoma on colonoscopy can range from a polyp to a fungating mass. In those with known malignant melanoma, surveillance is typically routine PET and CT scans. Whole-body FDG-PET/CTs have a 91% sensitivity and 92% specificity for detecting melanoma metastasis. Unfortunately for our patient no lesions were seen on PET two years prior or CT three months prior to colonoscopy. This case is an important reminder that for patients with a melanoma history one should consider the possibility of colonic metastasis both in asymptomatic screening colonoscopies and in symptomatic diagnostic colonoscopies.

Disclosures:
Rachael Schneider, DO, Stefanie Gallagher, DO, Amanda Long, DO, Marc Zitin, MD. P0215 - A Rare Case of Metastatic Melanoma to Cecum Found on Screening Colonoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Metastatic melanoma is the fifth most common cause of cancer in the United States. The 5-year survival of metastatic melanoma is about 25%. The most common sites of metastasis are skin, lungs, liver, and bone. Metastasis to the gastrointestinal (GI) tract accounts for just 1-3% of malignant melanomas with the small intestine and stomach being the most common sites. We present the case of a patient with stage IV melanoma found to have colonic metastasis on screening colonoscopy.
Case Description/Methods: Patient is a 76-year-old male with a history of hypertension, diabetes, coronary artery disease, and melanoma in situ of his right parietal scalp and left arm diagnosed in 2014. The melanomas were excised, and he received pembrolizumab from 2015 to 2016. He underwent radical resection for metastasis to the left upper back in 2019 and 2021. He underwent routine PET and CT scans for surveillance. CT in January 2023 noted no new lesions. His last screening colonoscopy was 12 years prior and recent hemoglobin was normal and he was without any GI complaints. He underwent screening colonoscopy in April 2023 showing a large cecal fungating and ulcerated mass involving half of the lumen circumference. Pathology confirmed metastatic melanoma of the colon. Stains positive for HMB-45, Melan A, Sox10. PET scan showed an FDG avid cecal mass with adjacent metastatic mesenteric nodes. He was seen by colorectal surgery and oncology. Given his lack of symptoms, decision made to hold off on surgery and start immunotherapy alone.
Discussion: Colonic metastases account for 15.5% of melanoma metastasis to the GI tract and 0.3% of melanoma metastasis overall. This rarity is due to the absence of melanocytes in the colon. Most cases of metastasis to the colon are diagnosed post-mortem as most patients are asymptomatic. The most common symptom is GI bleeding. Metastatic melanoma on colonoscopy can range from a polyp to a fungating mass. In those with known malignant melanoma, surveillance is typically routine PET and CT scans. Whole-body FDG-PET/CTs have a 91% sensitivity and 92% specificity for detecting melanoma metastasis. Unfortunately for our patient no lesions were seen on PET two years prior or CT three months prior to colonoscopy. This case is an important reminder that for patients with a melanoma history one should consider the possibility of colonic metastasis both in asymptomatic screening colonoscopies and in symptomatic diagnostic colonoscopies.

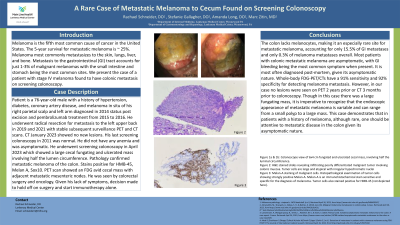
Figure: Figure 1: Colonoscope view of 6x4 cm fungated and ulcerated cecal mass, involving half the luminal circumference.
Figure 2: Melan-A staining of malignant cells. Histopathological examination of tumor cells showing strongly positive Melan-A. Melan-A is an immunohistochemical stain sensitive and specific for the diagnosis of melanoma. Tumor cells also stained positive for HMB-45 (not depicted here).
Figure 2: Melan-A staining of malignant cells. Histopathological examination of tumor cells showing strongly positive Melan-A. Melan-A is an immunohistochemical stain sensitive and specific for the diagnosis of melanoma. Tumor cells also stained positive for HMB-45 (not depicted here).
Disclosures:
Rachael Schneider indicated no relevant financial relationships.
Stefanie Gallagher indicated no relevant financial relationships.
Amanda Long indicated no relevant financial relationships.
Marc Zitin indicated no relevant financial relationships.
Rachael Schneider, DO, Stefanie Gallagher, DO, Amanda Long, DO, Marc Zitin, MD. P0215 - A Rare Case of Metastatic Melanoma to Cecum Found on Screening Colonoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
