Sunday Poster Session
Category: Colon
P0248 - Double Whammy: A Case Report of Immune Checkpoint Inhibitor Colitis and Concomitant CMV Colitis in a Patient on Nivolumab for Metastatic Melanoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Vinay Jahagirdar, MD
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Vinay Jahagirdar, MD1, Himil Mahadevia, MD1, Ronald Palmen, MD1, Kimberly Sanders, MD1, John Campbell, MD1, Pamela B. Sylvestre, MD2, Rajiv Chhabra, MD3, Wendell Clarkston, MD3, Sreeni S. Jonnalagadda, MD3
1University of Missouri-Kansas City, Kansas City, MO; 2Saint Luke’s Health System of Kansas City, Kansas City, MO; 3University of Missouri-Kansas City School of Medicine, Saint Luke’s Hospital of Kansas City, Kansas City, MO
Introduction: Immune checkpoint inhibitors (ICI) are the standard of care for numerous malignancies. They are associated with immune-related adverse effects, with the GI tract being most commonly affected. Agents including nivolumab and ipilimumab have been shown to cause diarrhea due to colitis and/or enteritis in up to 40% of patients.
Case Description/Methods: A 66-year-old male with a history of melanoma of the left face s/p Mohs surgery 7 years ago, presented to the ED with diarrhea. 6 months prior he was diagnosed with recurrent melanoma and cerebral metastasis, underwent resection, and was started on ICI therapy with ipilimumab/nivolumab and radiotherapy. After 2 cycles of ICI, he developed grade 2 diarrhea (4-6 stools/day). ICI was held and he was started on prednisone with suspicion for immune-mediated diarrhea.
After an initial response to steroids, diarrhea recurred, with ≥ 7 stools/day. Stool PCR was positive for Yersinia and colonic biopsies showed neutrophilic infiltrate, suggestive of active colitis of infectious etiology. The patient clinically improved after a course of ciprofloxacin.
Nivolumab was resumed, and 4 days later he presented to the ED with diarrhea that rapidly progressed to ~20 stools/day (severe/grade 4). Stool GI PCR panel and C. difficile PCR was negative. IV methylprednisolone was started. Repeat colonoscopy showed pan-colonic diffuse congestion, and erythema. A 5 mm sessile descending polyp was snared. Histology revealed active chronic colitis with mononuclear infiltrate and attenuation of the colonic epithelium, supporting the diagnosis of ICI colitis. Low-grade CMV colitis was detected by IHC, with presence of CMV-positive cells within the colon biopsy and polyp specimens.
The patient was started on a 3-week course of IV ganciclovir and Bactrim for PJP prophylaxis. He was discharged on a tapering course of prednisone 40 mg with plans to repeat sigmoidoscopy in 4-6 weeks to assess healing.
Discussion: Infectious etiology of diarrhea must be excluded before starting therapy for suspected ICI colitis. ICI colitis should be confirmed endoscopically before starting high-dose steroids. Systemic immunosuppression poses a risk of opportunistic infections and we found Yersinia and CMV in our patient on 2 different admissions. We wish to highlight the importance of excluding infectious etiologies before considering steroid failure in these patients. Infliximab and vedolizumab can be used in steroid-refractory cases, though caution must be employed in the setting of active infection.

Disclosures:
Vinay Jahagirdar, MD1, Himil Mahadevia, MD1, Ronald Palmen, MD1, Kimberly Sanders, MD1, John Campbell, MD1, Pamela B. Sylvestre, MD2, Rajiv Chhabra, MD3, Wendell Clarkston, MD3, Sreeni S. Jonnalagadda, MD3. P0248 - Double Whammy: A Case Report of Immune Checkpoint Inhibitor Colitis and Concomitant CMV Colitis in a Patient on Nivolumab for Metastatic Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2Saint Luke’s Health System of Kansas City, Kansas City, MO; 3University of Missouri-Kansas City School of Medicine, Saint Luke’s Hospital of Kansas City, Kansas City, MO
Introduction: Immune checkpoint inhibitors (ICI) are the standard of care for numerous malignancies. They are associated with immune-related adverse effects, with the GI tract being most commonly affected. Agents including nivolumab and ipilimumab have been shown to cause diarrhea due to colitis and/or enteritis in up to 40% of patients.
Case Description/Methods: A 66-year-old male with a history of melanoma of the left face s/p Mohs surgery 7 years ago, presented to the ED with diarrhea. 6 months prior he was diagnosed with recurrent melanoma and cerebral metastasis, underwent resection, and was started on ICI therapy with ipilimumab/nivolumab and radiotherapy. After 2 cycles of ICI, he developed grade 2 diarrhea (4-6 stools/day). ICI was held and he was started on prednisone with suspicion for immune-mediated diarrhea.
After an initial response to steroids, diarrhea recurred, with ≥ 7 stools/day. Stool PCR was positive for Yersinia and colonic biopsies showed neutrophilic infiltrate, suggestive of active colitis of infectious etiology. The patient clinically improved after a course of ciprofloxacin.
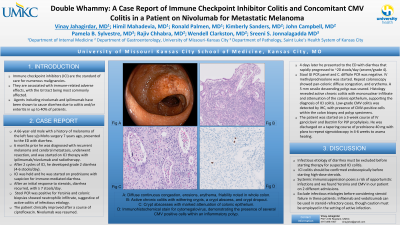
Nivolumab was resumed, and 4 days later he presented to the ED with diarrhea that rapidly progressed to ~20 stools/day (severe/grade 4). Stool GI PCR panel and C. difficile PCR was negative. IV methylprednisolone was started. Repeat colonoscopy showed pan-colonic diffuse congestion, and erythema. A 5 mm sessile descending polyp was snared. Histology revealed active chronic colitis with mononuclear infiltrate and attenuation of the colonic epithelium, supporting the diagnosis of ICI colitis. Low-grade CMV colitis was detected by IHC, with presence of CMV-positive cells within the colon biopsy and polyp specimens.
The patient was started on a 3-week course of IV ganciclovir and Bactrim for PJP prophylaxis. He was discharged on a tapering course of prednisone 40 mg with plans to repeat sigmoidoscopy in 4-6 weeks to assess healing.
Discussion: Infectious etiology of diarrhea must be excluded before starting therapy for suspected ICI colitis. ICI colitis should be confirmed endoscopically before starting high-dose steroids. Systemic immunosuppression poses a risk of opportunistic infections and we found Yersinia and CMV in our patient on 2 different admissions. We wish to highlight the importance of excluding infectious etiologies before considering steroid failure in these patients. Infliximab and vedolizumab can be used in steroid-refractory cases, though caution must be employed in the setting of active infection.

Figure: A: Diffuse continuous congestion, erosions, erythema, friability noted in whole colon. B: Active chronic colitis with withering crypts, a crypt abscess, and crypt dropout. C: Crypt abscesses with marked attenuation of colonic epithelium. D: Immunohistochemical stain for cytomegalovirus, demonstrating the presence of several CMV positive cells within an inflammatory polyp.
Disclosures:
Vinay Jahagirdar indicated no relevant financial relationships.
Himil Mahadevia indicated no relevant financial relationships.
Ronald Palmen indicated no relevant financial relationships.
Kimberly Sanders indicated no relevant financial relationships.
John Campbell indicated no relevant financial relationships.
Pamela B. Sylvestre indicated no relevant financial relationships.
Rajiv Chhabra indicated no relevant financial relationships.
Wendell Clarkston indicated no relevant financial relationships.
Sreeni S. Jonnalagadda indicated no relevant financial relationships.
Vinay Jahagirdar, MD1, Himil Mahadevia, MD1, Ronald Palmen, MD1, Kimberly Sanders, MD1, John Campbell, MD1, Pamela B. Sylvestre, MD2, Rajiv Chhabra, MD3, Wendell Clarkston, MD3, Sreeni S. Jonnalagadda, MD3. P0248 - Double Whammy: A Case Report of Immune Checkpoint Inhibitor Colitis and Concomitant CMV Colitis in a Patient on Nivolumab for Metastatic Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
