Sunday Poster Session
Category: Colon
P0258 - Mast Cell Colitis Associated With Yersinia Enterocolitica
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- OO
Olufemi E. Osikoya, MD
Medical City Arlington
Arlington, Texas
Presenting Author(s)
Gregory Brennan, MD1, Olufemi E. Osikoya, MD2
1Texas Digestive Disease Consultants, Mansfield, TX; 2Medical City Arlington, Arlington, TX
Introduction: Mast cells (MCs) have many functions including regulation of GI epithelial homeostasis, cross talk of the brain gut axis, host immune defenses, and inflammatory pathways. MCs are found in all layers of the GI tract and have been implicated in various gastrointestinal diseases. Although previously described in the literature, mast cell colitis is not considered a distinct clinical entity. This poses a challenge to the gastroenterologist who encounters such pathologic findings.
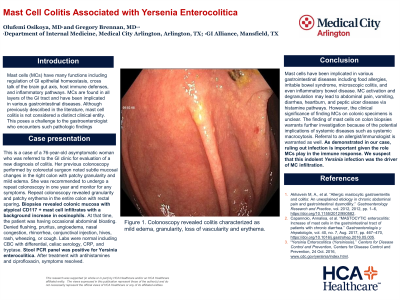
Case Description/Methods: This is a case of a 76-year-old woman who was referred to the gastroenterology clinic for evaluation of a new diagnosis of colitis. The patient had undergone a routine colonoscopy by a colorectal surgeon who had noted subtle mucosal changes in the right colon including patchy granularity and mild edema. The patient was asymptomatic, and therefore, it was recommended she undergo a repeat colonoscopy in one year and monitor for any symptoms. Repeat colonoscopy, one year later, revealed granularity and patchy erythema in the entire colon with rectal sparing. Biopsies revealed colonic mucosa with atypical CD117 + mast cell infiltrates with a background increase in eosinophils. At that time, the patient was having occasional abdominal bloating. She denied flushing, pruritus, angioedema, nasal congestion, rhinorrhea, conjunctival injection, hives, rash, wheezing, or cough. Laboratories were normal including CBC with differential, celiac serology, CRP, tryptase. Stool PCR panel was positive for Yersinia enterocolitica. The patient was treated with antihistamines and ciprofloxacin and her symptoms resolved.
Discussion: Mast cells have been implicated in various gastrointestinal diseases including food allergies, irritable bowel syndrome, microscopic colitis, and even inflammatory bowel disease. MC activation and degranulation may lead to abdominal pain, vomiting, diarrhea, heartburn, and peptic ulcer disease via histamine pathways. However, the clinical significance of finding MCs on colonic specimens is unclear. The finding of mast cells on colon biopsies warrants further investigation because of the potential implications of systemic diseases such as systemic macrocytosis. Referral to an allergist/immunologist is warranted as well. As demonstrated in our case, ruling out infection is important given the role MCs play in the immune response. We suspect that this indolent Yersinia infection was the driver of MC infiltration.

Disclosures:
Gregory Brennan, MD1, Olufemi E. Osikoya, MD2. P0258 - Mast Cell Colitis Associated With Yersinia Enterocolitica, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Digestive Disease Consultants, Mansfield, TX; 2Medical City Arlington, Arlington, TX
Introduction: Mast cells (MCs) have many functions including regulation of GI epithelial homeostasis, cross talk of the brain gut axis, host immune defenses, and inflammatory pathways. MCs are found in all layers of the GI tract and have been implicated in various gastrointestinal diseases. Although previously described in the literature, mast cell colitis is not considered a distinct clinical entity. This poses a challenge to the gastroenterologist who encounters such pathologic findings.
Case Description/Methods: This is a case of a 76-year-old woman who was referred to the gastroenterology clinic for evaluation of a new diagnosis of colitis. The patient had undergone a routine colonoscopy by a colorectal surgeon who had noted subtle mucosal changes in the right colon including patchy granularity and mild edema. The patient was asymptomatic, and therefore, it was recommended she undergo a repeat colonoscopy in one year and monitor for any symptoms. Repeat colonoscopy, one year later, revealed granularity and patchy erythema in the entire colon with rectal sparing. Biopsies revealed colonic mucosa with atypical CD117 + mast cell infiltrates with a background increase in eosinophils. At that time, the patient was having occasional abdominal bloating. She denied flushing, pruritus, angioedema, nasal congestion, rhinorrhea, conjunctival injection, hives, rash, wheezing, or cough. Laboratories were normal including CBC with differential, celiac serology, CRP, tryptase. Stool PCR panel was positive for Yersinia enterocolitica. The patient was treated with antihistamines and ciprofloxacin and her symptoms resolved.
Discussion: Mast cells have been implicated in various gastrointestinal diseases including food allergies, irritable bowel syndrome, microscopic colitis, and even inflammatory bowel disease. MC activation and degranulation may lead to abdominal pain, vomiting, diarrhea, heartburn, and peptic ulcer disease via histamine pathways. However, the clinical significance of finding MCs on colonic specimens is unclear. The finding of mast cells on colon biopsies warrants further investigation because of the potential implications of systemic diseases such as systemic macrocytosis. Referral to an allergist/immunologist is warranted as well. As demonstrated in our case, ruling out infection is important given the role MCs play in the immune response. We suspect that this indolent Yersinia infection was the driver of MC infiltration.

Figure: Colonoscopy revealed colitis characterized as mild edema, granularity, loss of vascularity and erythema.
Disclosures:
Gregory Brennan indicated no relevant financial relationships.
Olufemi Osikoya indicated no relevant financial relationships.
Gregory Brennan, MD1, Olufemi E. Osikoya, MD2. P0258 - Mast Cell Colitis Associated With Yersinia Enterocolitica, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
