Sunday Poster Session
Category: Colon
P0302 - Findings of Neuroendocrine Tumors in a Young Male with a Family History of Lynch Syndrome
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Shweta Bhatnagar, DO
McLaren Greater Lansing
Lansing, MI
Presenting Author(s)
Shweta Bhatnagar, DO, Alexandra Davies, DO, Jennifer Pryor, MD, Jennel Lee-Allen, MD
McLaren Greater Lansing, Lansing, MI
Introduction: Lynch syndrome (hereditary nonpolyposis colon cancer) is the most common cause of inherited cancer syndromes and is associated with elevated risks for colonic and extracolonic malignancies, earlier onset, and high rates of multiple primary cancers. Here is a case report highlighting findings of neuroendocrine tumors (NETs) in Lynch Syndrome.
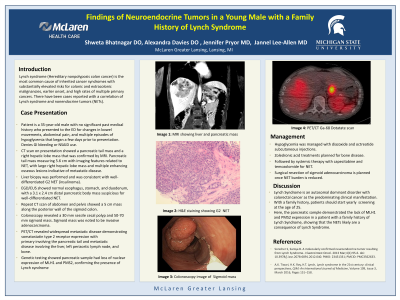
Case Description/Methods: Patient is a 35-year-old male with no significant medical history who presented to the ED for changes in bowel movements, abdominal pain, and multiple episodes of hypoglycemia that began a few days prior to presentation. He had a family history of Lynch Syndrome in his mother who was diagnosed with breast, uterine and colon cancer in her 40s. Patient did not start screening exams or complete genetics. CT scan in ED showed a pancreatic tail mass and a right hepatic lobe mass. MRI confirmed findings of a pancreatic tail mass with imaging features related to NET, large right hepatic lobe mass and multiple enhancing osseous lesions indicative of metastatic disease. Liver biopsy was consistent with well-differentiated G2 insulinoma. EUS showed a 3.1 x 2.4 cm distal pancreatic body mass suspicious for well-differentiated pancreatic NET. Patient's hospital course noted ongoing constipation. Repeat CT scan of abdomen and pelvis showed a 5 cm mass along the posterior wall of the sigmoid. Colonoscopy revealed a 30 mm sessile cecal polyp and 50-70mm sigmoid mass. Sigmoid mass was noted to be invasive adenocarcinoma. Genetic testing showed pancreatic sample had loss of nuclear expression of MLH1 and PMS2, confirming the presence of Lynch syndrome.
Discussion: Patient was discharged after stabilization of his blood glucose levels using diazoxide and underwent PET/CT Ga-68 dotatate scan which revealed widespread metastatic disease and somatostatin type 2 receptor expression with primary malignancy involving the pancreatic tail with metastatic disease involving the liver, left periaortic lymph node, axial and proximal appendicular skeleton. Treatment plans include management of hypoglycemia with diazoxide and octreotide subcutaneous injections, zoledronic acid for bone disease, and systemic therapy with capecitabine and temozolomide to decrease NET burden. Surgical resection of sigmoid adenocarcinoma to follow. Case above emphasizes early genetic testing and screening for Lynch Syndrome, as well as importance of multidisciplinary communication. This case also correlates findings of NET with genetically confirmed lynch syndrome.
Disclosures:
Shweta Bhatnagar, DO, Alexandra Davies, DO, Jennifer Pryor, MD, Jennel Lee-Allen, MD. P0302 - Findings of Neuroendocrine Tumors in a Young Male with a Family History of Lynch Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
McLaren Greater Lansing, Lansing, MI
Introduction: Lynch syndrome (hereditary nonpolyposis colon cancer) is the most common cause of inherited cancer syndromes and is associated with elevated risks for colonic and extracolonic malignancies, earlier onset, and high rates of multiple primary cancers. Here is a case report highlighting findings of neuroendocrine tumors (NETs) in Lynch Syndrome.
Case Description/Methods: Patient is a 35-year-old male with no significant medical history who presented to the ED for changes in bowel movements, abdominal pain, and multiple episodes of hypoglycemia that began a few days prior to presentation. He had a family history of Lynch Syndrome in his mother who was diagnosed with breast, uterine and colon cancer in her 40s. Patient did not start screening exams or complete genetics. CT scan in ED showed a pancreatic tail mass and a right hepatic lobe mass. MRI confirmed findings of a pancreatic tail mass with imaging features related to NET, large right hepatic lobe mass and multiple enhancing osseous lesions indicative of metastatic disease. Liver biopsy was consistent with well-differentiated G2 insulinoma. EUS showed a 3.1 x 2.4 cm distal pancreatic body mass suspicious for well-differentiated pancreatic NET. Patient's hospital course noted ongoing constipation. Repeat CT scan of abdomen and pelvis showed a 5 cm mass along the posterior wall of the sigmoid. Colonoscopy revealed a 30 mm sessile cecal polyp and 50-70mm sigmoid mass. Sigmoid mass was noted to be invasive adenocarcinoma. Genetic testing showed pancreatic sample had loss of nuclear expression of MLH1 and PMS2, confirming the presence of Lynch syndrome.
Discussion: Patient was discharged after stabilization of his blood glucose levels using diazoxide and underwent PET/CT Ga-68 dotatate scan which revealed widespread metastatic disease and somatostatin type 2 receptor expression with primary malignancy involving the pancreatic tail with metastatic disease involving the liver, left periaortic lymph node, axial and proximal appendicular skeleton. Treatment plans include management of hypoglycemia with diazoxide and octreotide subcutaneous injections, zoledronic acid for bone disease, and systemic therapy with capecitabine and temozolomide to decrease NET burden. Surgical resection of sigmoid adenocarcinoma to follow. Case above emphasizes early genetic testing and screening for Lynch Syndrome, as well as importance of multidisciplinary communication. This case also correlates findings of NET with genetically confirmed lynch syndrome.
Disclosures:
Shweta Bhatnagar indicated no relevant financial relationships.
Alexandra Davies indicated no relevant financial relationships.
Jennifer Pryor indicated no relevant financial relationships.
Jennel Lee-Allen indicated no relevant financial relationships.
Shweta Bhatnagar, DO, Alexandra Davies, DO, Jennifer Pryor, MD, Jennel Lee-Allen, MD. P0302 - Findings of Neuroendocrine Tumors in a Young Male with a Family History of Lynch Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
