Sunday Poster Session
Category: Colon
P0324 - Strongyloides Colitis: An Inflammatory Bowel Disease Imitator
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- EB
Edward Butt, MD, MPH
UTMB
Galveston, TX
Presenting Author(s)
Edward Butt, MD, MPH1, Ernesto Zamora, MD2, Nikita Garg, MD1, Yamam Al Saadi, MBBS2
1UTMB, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Strongyloides Stercoralis is a parasitic roundworm that is endemic to tropical and subtropical regions (1). The severity of disease can range from no symptoms to death (2). The non-specific and inconsistent findings associated with Strongyloidiasis are similar to inflammatory bowel disease (IBD) which may result in misdiagnosis. We herein present a case of strongyloides colitis.
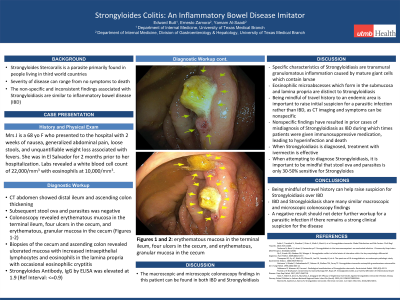
Case Description/Methods: A 68-year-old female with a past medical history of anxiety presented to the hospital with a 2-week history of nausea, generalized abdominal pain, loose stools, anorexia, weight loss and fever. She reported visiting El Salvador for 2 months prior to the onset of her symptoms. Blood workup was remarkable for a white blood cell count of 22,000/mm3 with eosinophilia at 10,000/mm3. CT scan of the abdomen showed distal ileum and ascending colon thickening. Multiple subsequent stool ova and parasites were negative. Colonoscopy revealed erythematous mucosa in the terminal ileum, multiple cratered ulcers in the cecum, and erythematous, granular mucosa in the cecum (Figures 1-2). Biopsies of the cecum and ascending colon revealed ulcerated mucosa with increased intraepithelial lymphocytes and eosinophils in the lamina propria with occasional eosinophilic cryptitis. QuantiFERON Gold was negative. A subsequent Strongyloides Antibody, IgG by ELISA was elevated at 1.9 (Ref Interval: < =0.9).
Discussion: The histomorphological and endoscopic findings of IBD and Strongyloidiasis can overlap (3, 4). Specific characteristics of Strongyloidiasis are transmural granulomatous inflammation caused by mature giant cells which contain larvae (3, 5). In addition, eosinophilic microabscesses which form in the submucosa and lamina propria are distinct to Strongyloidiasis (3).
Being mindful of travel history to an endemic area is important to raise initial suspicion for a parasitic infection rather than IBD. CT imaging findings and symptoms can be nonspecific (6). This has resulted in misdiagnosis of Strongyloidiasis as IBD. These patients were given immunosuppressive medication which exacerbated the disease, causing hyperinfection and death (7). Stool ova and parasites is only 30-50% sensitive for Strongyloides. Therefore, a negative result should not deter further workup for a parasitic infection if there remains a strong clinical suspicion for the disease (8). In cases where Strongyloidiasis is diagnosed, treatment with ivermectin shows effective results (9).

Disclosures:
Edward Butt, MD, MPH1, Ernesto Zamora, MD2, Nikita Garg, MD1, Yamam Al Saadi, MBBS2. P0324 - Strongyloides Colitis: An Inflammatory Bowel Disease Imitator, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UTMB, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Strongyloides Stercoralis is a parasitic roundworm that is endemic to tropical and subtropical regions (1). The severity of disease can range from no symptoms to death (2). The non-specific and inconsistent findings associated with Strongyloidiasis are similar to inflammatory bowel disease (IBD) which may result in misdiagnosis. We herein present a case of strongyloides colitis.
Case Description/Methods: A 68-year-old female with a past medical history of anxiety presented to the hospital with a 2-week history of nausea, generalized abdominal pain, loose stools, anorexia, weight loss and fever. She reported visiting El Salvador for 2 months prior to the onset of her symptoms. Blood workup was remarkable for a white blood cell count of 22,000/mm3 with eosinophilia at 10,000/mm3. CT scan of the abdomen showed distal ileum and ascending colon thickening. Multiple subsequent stool ova and parasites were negative. Colonoscopy revealed erythematous mucosa in the terminal ileum, multiple cratered ulcers in the cecum, and erythematous, granular mucosa in the cecum (Figures 1-2). Biopsies of the cecum and ascending colon revealed ulcerated mucosa with increased intraepithelial lymphocytes and eosinophils in the lamina propria with occasional eosinophilic cryptitis. QuantiFERON Gold was negative. A subsequent Strongyloides Antibody, IgG by ELISA was elevated at 1.9 (Ref Interval: < =0.9).
Discussion: The histomorphological and endoscopic findings of IBD and Strongyloidiasis can overlap (3, 4). Specific characteristics of Strongyloidiasis are transmural granulomatous inflammation caused by mature giant cells which contain larvae (3, 5). In addition, eosinophilic microabscesses which form in the submucosa and lamina propria are distinct to Strongyloidiasis (3).
Being mindful of travel history to an endemic area is important to raise initial suspicion for a parasitic infection rather than IBD. CT imaging findings and symptoms can be nonspecific (6). This has resulted in misdiagnosis of Strongyloidiasis as IBD. These patients were given immunosuppressive medication which exacerbated the disease, causing hyperinfection and death (7). Stool ova and parasites is only 30-50% sensitive for Strongyloides. Therefore, a negative result should not deter further workup for a parasitic infection if there remains a strong clinical suspicion for the disease (8). In cases where Strongyloidiasis is diagnosed, treatment with ivermectin shows effective results (9).

Figure: Ulcerations in the cecum
Disclosures:
Edward Butt indicated no relevant financial relationships.
Ernesto Zamora indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
Yamam Al Saadi indicated no relevant financial relationships.
Edward Butt, MD, MPH1, Ernesto Zamora, MD2, Nikita Garg, MD1, Yamam Al Saadi, MBBS2. P0324 - Strongyloides Colitis: An Inflammatory Bowel Disease Imitator, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
