Sunday Poster Session
Category: Colorectal Cancer Prevention
P0374 - Acute Hepatic Failure: Atypical Presentation of Metastatic Colorectal Cancer Not Detected by Imaging Studies
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Raj Jessica Thomas, DO
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Raj Jessica Thomas, DO, Olga Lytvynova, MD, Aijaz Sofi, MD
Cleveland Clinic Akron General, Akron, OH
Introduction: Diffuse parenchymal metastasis is a rare and occult pattern of liver metastasis that can lead to acute hepatic failure. Presented is a case of a 53 -year-old male with a past medical history significant for Stage IV colorectal adenocarcinoma (pT4bN2b) who presented with altered mentation, abnormal liver enzymes, and elevated total bilirubin. Doppler Ultrasound and Computed Tomography (CT) of the liver failed to detect any definite liver metastasis. Given worsening liver function tests (LFT), random liver biopsy was ultimately pursued confirming diagnosis of diffuse hepatic metastatic colorectal adenocarcinoma. The patient was transitioned to hospice and died four days later. To our knowledge, this is the first case of fulminant hepatic failure secondary to diffuse parenchymal liver infiltration from colorectal adenocarcinoma. This case stands as a reminder to the possibility of diffuse liver metastasis in the setting of acute hepatic failure even if imaging may be inconclusive.
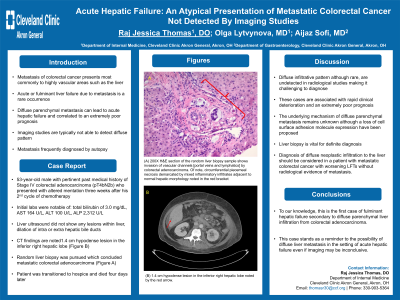
Case Description/Methods: A 53-year-old male with pertinent past medical history of Stage IV colorectal adenocarcinoma (pT4bN2b) with direct invasion to distal pancreas, status post: left colectomy, splenectomy, and distal pancreatectomy and metastasis to the bone, presents with altered mentation three weeks after his 2nd cycle of chemotherapy. Total bilirubin of 3.0 mg/dL, AST 164 U/L, ALT 100 U/L, ALP 2,312 U/L. Liver ultrasound did not show any lesions within liver, dilation of intra or extra hepatic bile ducts. CT was notable for: 1.4 cm hypodense lesion in the inferior right lobe (Figure 1B). Given progressive obstructive LFT pattern with no clear etiology and inconclusive imaging studies, a random liver biopsy was pursued which concluded metastatic colorectal adenocarcinoma (Figure 1A). Subsequently, patient was transitioned to hospice and died four days later.
Discussion: Given the vascular nature of the liver, there is a high propensity for metastasis to occur; diffuse infiltrative pattern, although rare, are undetected in radiological studies making it challenging to diagnose. These cases are associated with rapid clinical deterioration and extremely poor prognosis. Liver biopsy is vital for definite diagnosis. Diagnosis of diffuse neoplastic infiltration to the liver should be considered in a patient with metastatic colorectal cancer with worsening LFT without radiological evidence of metastasis.

Disclosures:
Raj Jessica Thomas, DO, Olga Lytvynova, MD, Aijaz Sofi, MD. P0374 - Acute Hepatic Failure: Atypical Presentation of Metastatic Colorectal Cancer Not Detected by Imaging Studies, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Cleveland Clinic Akron General, Akron, OH
Introduction: Diffuse parenchymal metastasis is a rare and occult pattern of liver metastasis that can lead to acute hepatic failure. Presented is a case of a 53 -year-old male with a past medical history significant for Stage IV colorectal adenocarcinoma (pT4bN2b) who presented with altered mentation, abnormal liver enzymes, and elevated total bilirubin. Doppler Ultrasound and Computed Tomography (CT) of the liver failed to detect any definite liver metastasis. Given worsening liver function tests (LFT), random liver biopsy was ultimately pursued confirming diagnosis of diffuse hepatic metastatic colorectal adenocarcinoma. The patient was transitioned to hospice and died four days later. To our knowledge, this is the first case of fulminant hepatic failure secondary to diffuse parenchymal liver infiltration from colorectal adenocarcinoma. This case stands as a reminder to the possibility of diffuse liver metastasis in the setting of acute hepatic failure even if imaging may be inconclusive.
Case Description/Methods: A 53-year-old male with pertinent past medical history of Stage IV colorectal adenocarcinoma (pT4bN2b) with direct invasion to distal pancreas, status post: left colectomy, splenectomy, and distal pancreatectomy and metastasis to the bone, presents with altered mentation three weeks after his 2nd cycle of chemotherapy. Total bilirubin of 3.0 mg/dL, AST 164 U/L, ALT 100 U/L, ALP 2,312 U/L. Liver ultrasound did not show any lesions within liver, dilation of intra or extra hepatic bile ducts. CT was notable for: 1.4 cm hypodense lesion in the inferior right lobe (Figure 1B). Given progressive obstructive LFT pattern with no clear etiology and inconclusive imaging studies, a random liver biopsy was pursued which concluded metastatic colorectal adenocarcinoma (Figure 1A). Subsequently, patient was transitioned to hospice and died four days later.
Discussion: Given the vascular nature of the liver, there is a high propensity for metastasis to occur; diffuse infiltrative pattern, although rare, are undetected in radiological studies making it challenging to diagnose. These cases are associated with rapid clinical deterioration and extremely poor prognosis. Liver biopsy is vital for definite diagnosis. Diagnosis of diffuse neoplastic infiltration to the liver should be considered in a patient with metastatic colorectal cancer with worsening LFT without radiological evidence of metastasis.

Figure: Figure 1: (A) 200X H&E section of the random liver biopsy sample shows invasion of vascular channels [portal veins and lymphatics] by colorectal adenocarcinoma. Of note, circumferential piecemeal necrosis demarcated by mixed inflammatory infiltrates adjacent to normal hepatic morphology noted in the red bracket. (B) 1.4 cm hypodense lesion in the inferior right hepatic lobe noted by the red arrow.
Disclosures:
Raj Jessica Thomas indicated no relevant financial relationships.
Olga Lytvynova indicated no relevant financial relationships.
Aijaz Sofi indicated no relevant financial relationships.
Raj Jessica Thomas, DO, Olga Lytvynova, MD, Aijaz Sofi, MD. P0374 - Acute Hepatic Failure: Atypical Presentation of Metastatic Colorectal Cancer Not Detected by Imaging Studies, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
