Sunday Poster Session
Category: Esophagus
P0455 - Granulosa Cell Tumor of the Proximal Esophagus – An Unusual Cause of Dysphagia
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Andrea R. Amaro, MD
University of Texas Southwestern Medical Center
Dallas, TX
Presenting Author(s)
Andrea R.. Amaro, MD1, Shaun McKenzie, MD2, Rafael Amaro, MD3
1University of Texas Southwestern Medical Center, Dallas, TX; 2Texas Oncology Surgical Specialists, Austin, TX; 3Texas Digestive Disease Consultants, Cedar Park, TX
Introduction: Granulosa cell tumors (GCT) are rare stromal tumors originating from Schwann cells that can occur virtually anywhere in the body. Approximately 5-8% arise in the gastrointestinal tract, with about 60% of these occurring in the esophagus. Here we present the case of a patient with chronic dysphagia who was found to have a proximal esophageal GCT.
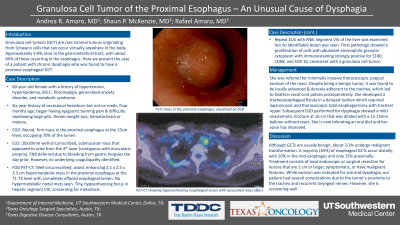
Case Description/Methods: A 60-year-old female with a past medical history of hypertension and hyperlipidemia presented with four months of epigastric burning pain and dysphagia. EGD revealed a firm submucosal mass in the proximal esophagus, occupying about 70% of the lumen. An FDG PET/CT scan showed a well-circumscribed, ovoid, enhancing, hypermetabolic mass at the proximal esophagus with mass effect. A small hypo-enhancing focus at hepatic segment VIII was seen, concerning for metastasis. No nodal metastases were seen. EUS demonstrated a 3.1 x 2 cm subepithelial hypoechoic mass about 18 cm from the incisors arising from the muscularis propria. Fine-needle biopsy was obtained which showed spindle cells on initial prep. Segment VIII of the liver was examined but no identifiable lesion was seen. Final pathology showed a proliferation of cells with abundant eosinophilic granular cytoplasm with immunostaining strongly positive for S100, CD68, and SOX 10, consistent with a granulosa cell tumor. She was referred for minimally invasive thoracoscopic surgical excision of the mass. Despite being a benign tumor, it was found to be locally advanced and densely adherent to the trachea, which led to bilateral vocal cord palsies postoperatively. She developed a tracheoesophageal fistula in a delayed fashion which required laparoscopic and thoracoscopic total esophagectomy with tracheal repair. Subsequent EGD performed for dysphagia showed a mild anastomotic stricture at 16 cm that was dilated with a 12-15mm balloon without tears. She is now tolerating an oral diet and her voice has improved.
Discussion: Although GCTs are usually benign, about 2-3% undergo malignant transformation. A majority (65%) of esophageal GCTs occur distally, with 20% in the mid-esophagus and only 15% proximally. Treatment consists of local endoscopic or surgical resection for lesions that are 1 cm or larger, symptomatic, or have malignant features. While excision was indicated for size and dysphagia, our patient had several complications due to the tumor’s proximity to the trachea and recurrent laryngeal nerves. However, she is recovering well.

Disclosures:
Andrea R.. Amaro, MD1, Shaun McKenzie, MD2, Rafael Amaro, MD3. P0455 - Granulosa Cell Tumor of the Proximal Esophagus – An Unusual Cause of Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Southwestern Medical Center, Dallas, TX; 2Texas Oncology Surgical Specialists, Austin, TX; 3Texas Digestive Disease Consultants, Cedar Park, TX
Introduction: Granulosa cell tumors (GCT) are rare stromal tumors originating from Schwann cells that can occur virtually anywhere in the body. Approximately 5-8% arise in the gastrointestinal tract, with about 60% of these occurring in the esophagus. Here we present the case of a patient with chronic dysphagia who was found to have a proximal esophageal GCT.
Case Description/Methods: A 60-year-old female with a past medical history of hypertension and hyperlipidemia presented with four months of epigastric burning pain and dysphagia. EGD revealed a firm submucosal mass in the proximal esophagus, occupying about 70% of the lumen. An FDG PET/CT scan showed a well-circumscribed, ovoid, enhancing, hypermetabolic mass at the proximal esophagus with mass effect. A small hypo-enhancing focus at hepatic segment VIII was seen, concerning for metastasis. No nodal metastases were seen. EUS demonstrated a 3.1 x 2 cm subepithelial hypoechoic mass about 18 cm from the incisors arising from the muscularis propria. Fine-needle biopsy was obtained which showed spindle cells on initial prep. Segment VIII of the liver was examined but no identifiable lesion was seen. Final pathology showed a proliferation of cells with abundant eosinophilic granular cytoplasm with immunostaining strongly positive for S100, CD68, and SOX 10, consistent with a granulosa cell tumor. She was referred for minimally invasive thoracoscopic surgical excision of the mass. Despite being a benign tumor, it was found to be locally advanced and densely adherent to the trachea, which led to bilateral vocal cord palsies postoperatively. She developed a tracheoesophageal fistula in a delayed fashion which required laparoscopic and thoracoscopic total esophagectomy with tracheal repair. Subsequent EGD performed for dysphagia showed a mild anastomotic stricture at 16 cm that was dilated with a 12-15mm balloon without tears. She is now tolerating an oral diet and her voice has improved.
Discussion: Although GCTs are usually benign, about 2-3% undergo malignant transformation. A majority (65%) of esophageal GCTs occur distally, with 20% in the mid-esophagus and only 15% proximally. Treatment consists of local endoscopic or surgical resection for lesions that are 1 cm or larger, symptomatic, or have malignant features. While excision was indicated for size and dysphagia, our patient had several complications due to the tumor’s proximity to the trachea and recurrent laryngeal nerves. However, she is recovering well.

Figure: Granulosa cell tumor of the proximal esophagus
Disclosures:
Andrea Amaro indicated no relevant financial relationships.
Shaun McKenzie indicated no relevant financial relationships.
Rafael Amaro indicated no relevant financial relationships.
Andrea R.. Amaro, MD1, Shaun McKenzie, MD2, Rafael Amaro, MD3. P0455 - Granulosa Cell Tumor of the Proximal Esophagus – An Unusual Cause of Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
