Sunday Poster Session
Category: General Endoscopy
P0561 - Iatrogenic Esophageal Perforations and Their Management
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Augustin R. Attwell, MD
University of Colorado Medical School
Denver, CO
Presenting Author(s)
Augustin R. Attwell, MD, Eric Montminy, MD
University of Colorado Medical School, Aurora, CO
Introduction: Iatrogenic esophageal perforation (IEP) is a severe adverse event (AE) of upper endoscopy procedures (UEPs) associated with severe morbidity. The management has shifted from surgery to endotherapy with clip placement (CP), self-expanding metal stent (SEMS), and vacuum therapy (VT), but the outcomes are variable and specific studies of IEP are limited.
Methods: IEPs associated with EGD, upper EUS, small bowel enteroscopy (SBE), and ERCP at the University of Colorado Hospital, Denver VA Medical Center, and Denver Health Medical Center from January 2010 to December 2022 were identified retrospectively from the AE database. Demographic, clinical, and procedural information including treatments and outcomes were obtained from the medical record. Statistical analysis was performed using Microsoft Excel and STATA.
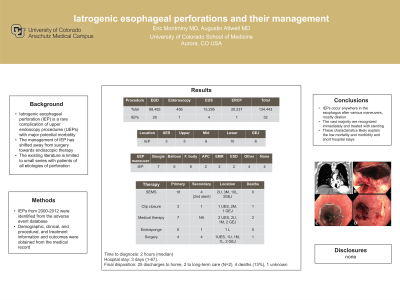
Results: Thirty-two IEPs from 26 EGDs, 4 EUS, 1 SBE, and 1 ERCP were identified. Seventeen cases (53%) involved a trainee and 28 cases occurred after foreign body removal (N=6), bougie dilation (N=7), balloon dilation (N=5) argon plasma coagulation (N=2), mucosal resection (N=2), submucosal dissection (N=2), fine-needle aspiration (N=2), large polyp extraction (N=1), and SEMS extraction (N=1). Location of IEP included the inlet (N=3); upper (N=5), middle (N=6), or lower (N=10) esophagus; and gastroesophageal junction (N=8). The diagnosis of IEP was diagnosed at a median of 2 hours (0.5 -168) after the injury by endoscopy (N=14), CT scan (N=12), esophagram (N=5), or x-ray (N=1). The initial treatment included conservative medical therapy (nil-per-os and IV antibiotics) alone (N=7), CP (N=3), SEMS placement (N=15), SEMS plus EP (N=3), primary surgical repair with or without gastrostomy tube placement (GTP, N=3), and video-assisted thoracoscopic surgery (N=1). Additional treatments were required in 11 patients including repeat CP (N=1), VT (N=1), repeat SEMS placement or adjustment (N=4), thoracoscopy or chest tube placement (N=3), or GTP (N=1). The median hospital stay was 3 days (1-67). Final disposition included discharge to home (N=25) or a long-term care facility (N=2), 4 deaths (13%), and 1 unknown (patient was discharged against medical advice).
Discussion: IEPs are rare nowadays but may occur anywhere in the esophagus and after any UEP, typically with therapeutic intervention. The vast majority are recognized immediately and managed endoscopically, and these characteristics likely explain the short hospitalization and low mortality.

Disclosures:
Augustin R. Attwell, MD, Eric Montminy, MD. P0561 - Iatrogenic Esophageal Perforations and Their Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Colorado Medical School, Aurora, CO
Introduction: Iatrogenic esophageal perforation (IEP) is a severe adverse event (AE) of upper endoscopy procedures (UEPs) associated with severe morbidity. The management has shifted from surgery to endotherapy with clip placement (CP), self-expanding metal stent (SEMS), and vacuum therapy (VT), but the outcomes are variable and specific studies of IEP are limited.
Methods: IEPs associated with EGD, upper EUS, small bowel enteroscopy (SBE), and ERCP at the University of Colorado Hospital, Denver VA Medical Center, and Denver Health Medical Center from January 2010 to December 2022 were identified retrospectively from the AE database. Demographic, clinical, and procedural information including treatments and outcomes were obtained from the medical record. Statistical analysis was performed using Microsoft Excel and STATA.
Results: Thirty-two IEPs from 26 EGDs, 4 EUS, 1 SBE, and 1 ERCP were identified. Seventeen cases (53%) involved a trainee and 28 cases occurred after foreign body removal (N=6), bougie dilation (N=7), balloon dilation (N=5) argon plasma coagulation (N=2), mucosal resection (N=2), submucosal dissection (N=2), fine-needle aspiration (N=2), large polyp extraction (N=1), and SEMS extraction (N=1). Location of IEP included the inlet (N=3); upper (N=5), middle (N=6), or lower (N=10) esophagus; and gastroesophageal junction (N=8). The diagnosis of IEP was diagnosed at a median of 2 hours (0.5 -168) after the injury by endoscopy (N=14), CT scan (N=12), esophagram (N=5), or x-ray (N=1). The initial treatment included conservative medical therapy (nil-per-os and IV antibiotics) alone (N=7), CP (N=3), SEMS placement (N=15), SEMS plus EP (N=3), primary surgical repair with or without gastrostomy tube placement (GTP, N=3), and video-assisted thoracoscopic surgery (N=1). Additional treatments were required in 11 patients including repeat CP (N=1), VT (N=1), repeat SEMS placement or adjustment (N=4), thoracoscopy or chest tube placement (N=3), or GTP (N=1). The median hospital stay was 3 days (1-67). Final disposition included discharge to home (N=25) or a long-term care facility (N=2), 4 deaths (13%), and 1 unknown (patient was discharged against medical advice).
Discussion: IEPs are rare nowadays but may occur anywhere in the esophagus and after any UEP, typically with therapeutic intervention. The vast majority are recognized immediately and managed endoscopically, and these characteristics likely explain the short hospitalization and low mortality.

Figure: Large IEP at the GE junction diagnosed by CT scan (A), confirmed by EGD (B), treated with SEMS placement (C), and healing confirmed by EGD 6 weeks later (D)
Disclosures:
Augustin Attwell indicated no relevant financial relationships.
Eric Montminy indicated no relevant financial relationships.
Augustin R. Attwell, MD, Eric Montminy, MD. P0561 - Iatrogenic Esophageal Perforations and Their Management, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
