Sunday Poster Session
Category: GI Bleeding
P0621 - Multiple Myeloma Presenting as Gastrointestinal Bleeding From Gastric Amyloidosis: A Case Report
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Marc Hersh, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Marc Hersh, MD1, Gabriel J. Dinatale, MD1, Juan P. Palazzo, MD1, Monjur Ahmed, MD, FACG2
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Thomas Jefferson University, Philadelphia, PA
Introduction: Gastric amyloidosis is an overall rare cause of gastrointestinal bleeding that is often poorly recognized in the clinical setting. It is estimated that the digestive system is affected in 3.2% of patients diagnosed with amyloidosis but in 10% of patients with the primary (AL) subtype. We present a relatively unusual case of multiple myeloma presenting as gastrointestinal amyloidosis with gastrointestinal bleed.
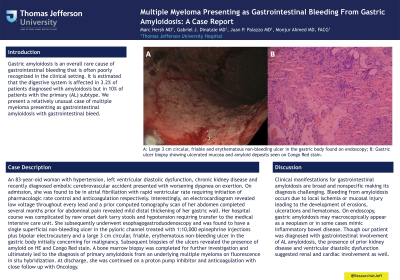
Case Description/Methods: An 83-year-old woman with hypertension, left ventricular diastolic dysfunction, chronic kidney disease and recently diagnosed embolic cerebrovascular accident presented with worsening dyspnea on exertion. On admission, she was found to be in atrial fibrillation with rapid ventricular rate requiring initiation of pharmacologic rate control and anticoagulation respectively. Interestingly, an electrocardiogram revealed low voltage throughout every lead and a prior computed tomography scan of her abdomen completed several months prior for abdominal pain revealed mild distal thickening of her gastric wall. Her hospital course was complicated by new onset dark tarry stools and hypotension requiring transfer to the medical intensive care unit. She subsequently underwent esophagogastroduodenoscopy and was found to have a single superficial non-bleeding ulcer in the pyloric channel treated with 1:10,000 epinephrine injections plus bipolar electrocautery and a large 3 cm circular, friable, erythematous non-bleeding ulcer in the gastric body initially concerning for malignancy. Subsequent biopsies of the ulcers revealed the presence of amyloid on HE and Congo Red stain. A bone marrow biopsy was completed for further investigation and ultimately led to the diagnosis of primary amyloidosis from an underlying multiple myeloma on fluorescence in situ hybridization. At discharge, she was continued on a proton pump inhibitor and anticoagulation with close follow up with Oncology.
Discussion: Clinical manifestations for gastrointestinal amyloidosis are broad and nonspecific making its diagnosis challenging. Bleeding from amyloidosis occurs due to local ischemia or mucosal injury leading to the development of erosions, ulcerations and hematomas. On endoscopy, gastric amyloidosis may macroscopically appear as a neoplasm or in some cases mimic inflammatory bowel disease. Though our patient was diagnosed with gastrointestinal involvement of AL amyloidosis, the presence of prior kidney disease and ventricular diastolic dysfunction suggested renal and cardiac involvement as well.

Disclosures:
Marc Hersh, MD1, Gabriel J. Dinatale, MD1, Juan P. Palazzo, MD1, Monjur Ahmed, MD, FACG2. P0621 - Multiple Myeloma Presenting as Gastrointestinal Bleeding From Gastric Amyloidosis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Thomas Jefferson University, Philadelphia, PA
Introduction: Gastric amyloidosis is an overall rare cause of gastrointestinal bleeding that is often poorly recognized in the clinical setting. It is estimated that the digestive system is affected in 3.2% of patients diagnosed with amyloidosis but in 10% of patients with the primary (AL) subtype. We present a relatively unusual case of multiple myeloma presenting as gastrointestinal amyloidosis with gastrointestinal bleed.
Case Description/Methods: An 83-year-old woman with hypertension, left ventricular diastolic dysfunction, chronic kidney disease and recently diagnosed embolic cerebrovascular accident presented with worsening dyspnea on exertion. On admission, she was found to be in atrial fibrillation with rapid ventricular rate requiring initiation of pharmacologic rate control and anticoagulation respectively. Interestingly, an electrocardiogram revealed low voltage throughout every lead and a prior computed tomography scan of her abdomen completed several months prior for abdominal pain revealed mild distal thickening of her gastric wall. Her hospital course was complicated by new onset dark tarry stools and hypotension requiring transfer to the medical intensive care unit. She subsequently underwent esophagogastroduodenoscopy and was found to have a single superficial non-bleeding ulcer in the pyloric channel treated with 1:10,000 epinephrine injections plus bipolar electrocautery and a large 3 cm circular, friable, erythematous non-bleeding ulcer in the gastric body initially concerning for malignancy. Subsequent biopsies of the ulcers revealed the presence of amyloid on HE and Congo Red stain. A bone marrow biopsy was completed for further investigation and ultimately led to the diagnosis of primary amyloidosis from an underlying multiple myeloma on fluorescence in situ hybridization. At discharge, she was continued on a proton pump inhibitor and anticoagulation with close follow up with Oncology.
Discussion: Clinical manifestations for gastrointestinal amyloidosis are broad and nonspecific making its diagnosis challenging. Bleeding from amyloidosis occurs due to local ischemia or mucosal injury leading to the development of erosions, ulcerations and hematomas. On endoscopy, gastric amyloidosis may macroscopically appear as a neoplasm or in some cases mimic inflammatory bowel disease. Though our patient was diagnosed with gastrointestinal involvement of AL amyloidosis, the presence of prior kidney disease and ventricular diastolic dysfunction suggested renal and cardiac involvement as well.

Figure: A: Large 3 cm circular, friable and erythematous non-bleeding ulcer in the gastric body found on endoscopy; B: Gastric ulcer biopsy showing ulcerated mucosa and amyloid deposits seen on Congo Red stain.
Disclosures:
Marc Hersh indicated no relevant financial relationships.
Gabriel Dinatale indicated no relevant financial relationships.
Juan Palazzo indicated no relevant financial relationships.
Monjur Ahmed indicated no relevant financial relationships.
Marc Hersh, MD1, Gabriel J. Dinatale, MD1, Juan P. Palazzo, MD1, Monjur Ahmed, MD, FACG2. P0621 - Multiple Myeloma Presenting as Gastrointestinal Bleeding From Gastric Amyloidosis: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
