Sunday Poster Session
Category: GI Bleeding
P0628 - Rectal Dieulafoy Lesion: A Rare Finding with Deadly Consequences
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Ussama Ghumman, MD
Bayhealth Medical Center
Dover, DE
Presenting Author(s)
Ussama Ghumman, MD1, Dipam Shah, MD2, Phi Tran, DO3, Haider Ghumman, MPH4, Vineet Gudsoorkar, MD1
1Bayhealth Medical Center, Dover, DE; 2INOVA Fairfax Hospital, Fairfax, VA; 3Baylor Scott & White, Temple, TX; 4University of Florida Morsani College of Medicine, Tampa, FL
Introduction: Dieulafoy’s lesion (DL), defined as a dilated submucosal vessel that erodes the overlying epithelium without evidence of a primary ulcer or erosion, is a rare cause of GI bleeding. Only 101 cases of rectal DL have been identified in the world literature so far. Here, we present a case of recurrent hematochezia from a rectal DL underscoring the challenges associated with this diagnosis
Case Description/Methods: A 45-year-old male on anticoagulation due to a mechanical aortic valve presented to the ER with acute painless hematochezia. He had no associated symptoms, was hemodynamically stable and had a normal abdominal examination. Rectal exam revealed bright red stool. Labs showed hemoglobin of 12.1g/dL, INR of 1.34 and normal metabolic panel. Ileocolonoscopy showed small non-bleeding internal hemorrhoids. A tagged RBC scan was negative for active bleeding. Hematochezia resolved and the patient was discharged on warfarin.
The patient returned after 3 months with the same presentation and supratherapeutic INR. Rectal exam showed active oozing in the distal rectum without mucosal lesion. The patient was discharged following suture ligation.
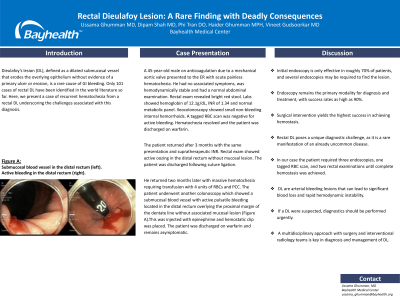
He returned two months later with massive hematochezia requiring transfusion with 4 units of RBCs and PCC. The patient underwent another colonoscopy which showed a submucosal blood vessel with active pulsatile bleeding located in the distal rectum overlying the proximal margin of the dentate line without associated mucosal lesion (Figure).This was injected with epinephrine and hemostatic clip was placed. The patient was discharged on warfarin and remains asymptomatic.
Discussion: DL is a rare cause of gastrointestinal bleeding. Initial endoscopy is only effective in roughly 70% of patients, and several endoscopies may be required to find the lesion. Endoscopy remains the primary modality for diagnosis and treatment, with success rates as high as 90%. Surgical intervention yields the highest success in achieving hemostasis. Rectal DL poses a unique diagnostic challenge, as it is a rare manifestation of an already uncommon disease. In our case the patient required three endoscopies, one tagged RBC scan, and two rectal examinations until complete hemostasis was achieved. DL are arterial bleeding lesions that can lead to significant blood loss and rapid hemodynamic instability. If a DL were suspected, diagnostics should be performed urgently. A multidisciplinary approach with surgery and interventional radiology teams is key in diagnosis and management of DL.

Disclosures:
Ussama Ghumman, MD1, Dipam Shah, MD2, Phi Tran, DO3, Haider Ghumman, MPH4, Vineet Gudsoorkar, MD1. P0628 - Rectal Dieulafoy Lesion: A Rare Finding with Deadly Consequences, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Bayhealth Medical Center, Dover, DE; 2INOVA Fairfax Hospital, Fairfax, VA; 3Baylor Scott & White, Temple, TX; 4University of Florida Morsani College of Medicine, Tampa, FL
Introduction: Dieulafoy’s lesion (DL), defined as a dilated submucosal vessel that erodes the overlying epithelium without evidence of a primary ulcer or erosion, is a rare cause of GI bleeding. Only 101 cases of rectal DL have been identified in the world literature so far. Here, we present a case of recurrent hematochezia from a rectal DL underscoring the challenges associated with this diagnosis
Case Description/Methods: A 45-year-old male on anticoagulation due to a mechanical aortic valve presented to the ER with acute painless hematochezia. He had no associated symptoms, was hemodynamically stable and had a normal abdominal examination. Rectal exam revealed bright red stool. Labs showed hemoglobin of 12.1g/dL, INR of 1.34 and normal metabolic panel. Ileocolonoscopy showed small non-bleeding internal hemorrhoids. A tagged RBC scan was negative for active bleeding. Hematochezia resolved and the patient was discharged on warfarin.
The patient returned after 3 months with the same presentation and supratherapeutic INR. Rectal exam showed active oozing in the distal rectum without mucosal lesion. The patient was discharged following suture ligation.
He returned two months later with massive hematochezia requiring transfusion with 4 units of RBCs and PCC. The patient underwent another colonoscopy which showed a submucosal blood vessel with active pulsatile bleeding located in the distal rectum overlying the proximal margin of the dentate line without associated mucosal lesion (Figure).This was injected with epinephrine and hemostatic clip was placed. The patient was discharged on warfarin and remains asymptomatic.
Discussion: DL is a rare cause of gastrointestinal bleeding. Initial endoscopy is only effective in roughly 70% of patients, and several endoscopies may be required to find the lesion. Endoscopy remains the primary modality for diagnosis and treatment, with success rates as high as 90%. Surgical intervention yields the highest success in achieving hemostasis. Rectal DL poses a unique diagnostic challenge, as it is a rare manifestation of an already uncommon disease. In our case the patient required three endoscopies, one tagged RBC scan, and two rectal examinations until complete hemostasis was achieved. DL are arterial bleeding lesions that can lead to significant blood loss and rapid hemodynamic instability. If a DL were suspected, diagnostics should be performed urgently. A multidisciplinary approach with surgery and interventional radiology teams is key in diagnosis and management of DL.

Figure: Figure: Submucosal blood vessel in the distal rectum (left). Active bleeding in the distal rectum (right).
Disclosures:
Ussama Ghumman indicated no relevant financial relationships.
Dipam Shah indicated no relevant financial relationships.
Phi Tran indicated no relevant financial relationships.
Haider Ghumman indicated no relevant financial relationships.
Vineet Gudsoorkar indicated no relevant financial relationships.
Ussama Ghumman, MD1, Dipam Shah, MD2, Phi Tran, DO3, Haider Ghumman, MPH4, Vineet Gudsoorkar, MD1. P0628 - Rectal Dieulafoy Lesion: A Rare Finding with Deadly Consequences, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
