Sunday Poster Session
Category: GI Bleeding
P0631 - A Rare Case of Double Pylorus in an Elderly Female
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- CC
Chanelle Chua, MD
Medical College of Wisconsin
Wauwatosa, WI
Presenting Author(s)
Chanelle Chua, MD1, Harpreet Singh, MD2, Paraj Patel, MD3, Sam Samuel, MD, PhD4
1Medical College of Wisconsin, Wauwatosa, WI; 2Medical College of Wisconsin, Milwaukee, WI; 3Clement J. Zablocki VA Medical Center, Milwaukee, WI; 4Sparks M. Matsunaga VA Medical Center, Honolulu, HI
Introduction: Peptic ulcer disease (PUD) is a common diagnosis associated with two main risk factors: H. pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs). Despite the declining incidence of PUD, its associated complications are more prevalent in the elderly. Rarely, PUD can result in the formation of a fistula between gastric body and duodenum or acquired double pylorus (ADP). Here we report a case of ADP in an elderly woman on high dose aspirin therapy.
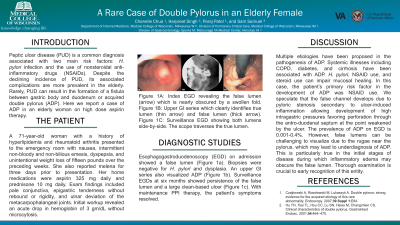
Case Description/Methods: A 71-year-old woman with a history of hyperlipidemia and rheumatoid arthritis presented to the emergency room with nausea, intermittent non-bloody and non-bilious emesis, dyspepsia, and unintentional weight loss of fifteen pounds over the preceding weeks. She also reported melena for three days prior to presentation. Her home medications were aspirin 325 mg daily and prednisone 10 mg daily. Exam findings included pale conjunctiva, epigastric tenderness without rebound or rigidity, and ulnar deviation of the metacarpophalangeal joints. Initial workup revealed an acute drop in hemoglobin of 3 gm/dL without microcytosis. Esophagogastroduodenoscopy (EGD) on admission showed a false lumen (Figure 1a). Biopsies were negative for H. pylori and dysplasia. An upper GI series also visualized ADP (Figure 1b). Surveillance EGDs at six months showed persistence of the false lumen and a large clean-based ulcer (Figure 1c). With maintenance PPI therapy, the patient’s symptoms resolved.
Discussion: Multiple etiologies have been proposed in the pathogenesis of ADP. Systemic illnesses including chronic obstructive pulmonary disease, diabetes, and cirrhosis have been associated with ADP. H. pylori, NSAID use, and corticosteroid use can impair mucosal healing. In this case, the patient’s primary risk factor in the development of ADP was NSAID use. We speculate that the false channel develops due to pyloric stenosis secondary to ulcer-induced inflammation allowing the development of high intragastric pressures favoring perforation through the antro-duodenal septum at the point weakened by the ulcer. The prevalence of ADP on EGD is between 0.001 and 0.4%. However, false lumens can be challenging to visualize due to the rugae and folds located near the pylorus, which may lead to underdiagnosis of ADP. This is particularly true in the initial stages of disease during which inflammatory edema may obscure the false lumen. Thorough examination is crucial to early recognition of this entity.

Disclosures:
Chanelle Chua, MD1, Harpreet Singh, MD2, Paraj Patel, MD3, Sam Samuel, MD, PhD4. P0631 - A Rare Case of Double Pylorus in an Elderly Female, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Medical College of Wisconsin, Wauwatosa, WI; 2Medical College of Wisconsin, Milwaukee, WI; 3Clement J. Zablocki VA Medical Center, Milwaukee, WI; 4Sparks M. Matsunaga VA Medical Center, Honolulu, HI
Introduction: Peptic ulcer disease (PUD) is a common diagnosis associated with two main risk factors: H. pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs). Despite the declining incidence of PUD, its associated complications are more prevalent in the elderly. Rarely, PUD can result in the formation of a fistula between gastric body and duodenum or acquired double pylorus (ADP). Here we report a case of ADP in an elderly woman on high dose aspirin therapy.
Case Description/Methods: A 71-year-old woman with a history of hyperlipidemia and rheumatoid arthritis presented to the emergency room with nausea, intermittent non-bloody and non-bilious emesis, dyspepsia, and unintentional weight loss of fifteen pounds over the preceding weeks. She also reported melena for three days prior to presentation. Her home medications were aspirin 325 mg daily and prednisone 10 mg daily. Exam findings included pale conjunctiva, epigastric tenderness without rebound or rigidity, and ulnar deviation of the metacarpophalangeal joints. Initial workup revealed an acute drop in hemoglobin of 3 gm/dL without microcytosis. Esophagogastroduodenoscopy (EGD) on admission showed a false lumen (Figure 1a). Biopsies were negative for H. pylori and dysplasia. An upper GI series also visualized ADP (Figure 1b). Surveillance EGDs at six months showed persistence of the false lumen and a large clean-based ulcer (Figure 1c). With maintenance PPI therapy, the patient’s symptoms resolved.
Discussion: Multiple etiologies have been proposed in the pathogenesis of ADP. Systemic illnesses including chronic obstructive pulmonary disease, diabetes, and cirrhosis have been associated with ADP. H. pylori, NSAID use, and corticosteroid use can impair mucosal healing. In this case, the patient’s primary risk factor in the development of ADP was NSAID use. We speculate that the false channel develops due to pyloric stenosis secondary to ulcer-induced inflammation allowing the development of high intragastric pressures favoring perforation through the antro-duodenal septum at the point weakened by the ulcer. The prevalence of ADP on EGD is between 0.001 and 0.4%. However, false lumens can be challenging to visualize due to the rugae and folds located near the pylorus, which may lead to underdiagnosis of ADP. This is particularly true in the initial stages of disease during which inflammatory edema may obscure the false lumen. Thorough examination is crucial to early recognition of this entity.

Figure: Figure 1A: Index EGD revealing the false lumen (arrow) which is nearly obscured by a swollen fold.
Figure 1B: Upper GI series which clearly identifies true lumen (thin arrow) and false lumen (thick arrow).
Figure 1C: Surveillance EGD showing both lumens side-by-side. The scope traverses the true lumen.
Figure 1B: Upper GI series which clearly identifies true lumen (thin arrow) and false lumen (thick arrow).
Figure 1C: Surveillance EGD showing both lumens side-by-side. The scope traverses the true lumen.
Disclosures:
Chanelle Chua indicated no relevant financial relationships.
Harpreet Singh indicated no relevant financial relationships.
Paraj Patel indicated no relevant financial relationships.
Sam Samuel indicated no relevant financial relationships.
Chanelle Chua, MD1, Harpreet Singh, MD2, Paraj Patel, MD3, Sam Samuel, MD, PhD4. P0631 - A Rare Case of Double Pylorus in an Elderly Female, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
