Sunday Poster Session
Category: GI Bleeding
P0640 - Malignant Melanoma Presenting With Upper Gastrointestinal Bleeding!
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Maxim Kostyk, DO
University Hospitals Parma
Parma, OH
Presenting Author(s)
Maxim Kostyk, DO1, Kevin Koch, DO1, Fady G. Haddad, MD2
1University Hospitals Parma, Parma, OH; 2University Hospitals, Parma, OH
Introduction: Malignant melanoma is an aggressive tumor that mostly originates from the skin. Despite that melanoma is the most common tumor to metastasize to the gastrointestinal (GI) tract, primary GI melanoma notably gastric melanoma is extremely rare and accounts for < 1% of melanoma cases. Even though primary or metastatic GI involvement by melanoma is well described, it is quite uncommon for melanoma to initially present with GI bleeding with only few cases reported in the literature. Herein we report the case of a 68 year-old patient presenting with hemorrhagic shock secondary to gastric malignant melanoma.
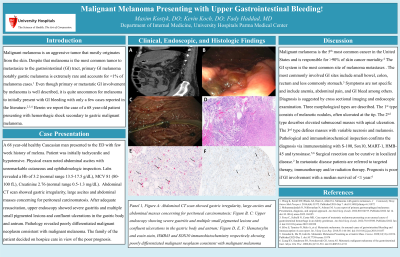
Case Description/Methods: A 68 year-old healthy Caucasian man presented to the ED with few week history of melena. Patient was initially tachycardic and hypotensive. Physical exam noted abdominal ascites with unremarkable cutaneous and ophthalmologic inspection. Labs revealed a Hb of 3.2 (normal range 13.5-17.5 g/dL), MCV 81 (80-100 fL), Creatinine 2.76 (normal range 0.5-1.3 mg/dL). Abdominal CT scan showed gastric irregularity, large ascites and abdominal masses concerning for peritoneal carcinomatosis. After adequate resuscitation, upper endoscopy showed severe gastritis and multiple small pigmented lesions and confluent ulcerations in the gastric body and antrum. Pathology revealed poorly differentiated malignant neoplasm consistent with malignant melanoma. Patient’s family decided on hospice care in view of the poor prognosis.
Discussion: Malignant melanoma is the 5th most common cancer in the United States and is responsible for >90% of skin cancer mortality. The GI system is the most common site of melanoma metastases . The most commonly involved GI sites include small bowel, colon, rectum and less commonly stomach. Symptoms are not specific and includes anemia, abdominal pain, GI bleed among others. Diagnosis is suggested by cross sectional imaging and endoscopic examination. Three morphological types are described. The 1st type consists of melanotic nodules, often ulcerated at the tip. The 2nd type describes elevated submucosal masses with apical ulceration. The 3rd type defines masses with variable necrosis and melanosis. Pathological and immunohistochemical inspection confirms the diagnosis via immunostaining with S-100, Sox10, MART-1, HMB-45 and tyrosinase. Surgical resection can be curative in localized disease. In metastatic disease patients are referred to targeted therapy, immunotherapy and/or radiation therapy. Prognosis is poor if GI involvement with a median survival of < 1 year.

Disclosures:
Maxim Kostyk, DO1, Kevin Koch, DO1, Fady G. Haddad, MD2. P0640 - Malignant Melanoma Presenting With Upper Gastrointestinal Bleeding!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University Hospitals Parma, Parma, OH; 2University Hospitals, Parma, OH
Introduction: Malignant melanoma is an aggressive tumor that mostly originates from the skin. Despite that melanoma is the most common tumor to metastasize to the gastrointestinal (GI) tract, primary GI melanoma notably gastric melanoma is extremely rare and accounts for < 1% of melanoma cases. Even though primary or metastatic GI involvement by melanoma is well described, it is quite uncommon for melanoma to initially present with GI bleeding with only few cases reported in the literature. Herein we report the case of a 68 year-old patient presenting with hemorrhagic shock secondary to gastric malignant melanoma.
Case Description/Methods: A 68 year-old healthy Caucasian man presented to the ED with few week history of melena. Patient was initially tachycardic and hypotensive. Physical exam noted abdominal ascites with unremarkable cutaneous and ophthalmologic inspection. Labs revealed a Hb of 3.2 (normal range 13.5-17.5 g/dL), MCV 81 (80-100 fL), Creatinine 2.76 (normal range 0.5-1.3 mg/dL). Abdominal CT scan showed gastric irregularity, large ascites and abdominal masses concerning for peritoneal carcinomatosis. After adequate resuscitation, upper endoscopy showed severe gastritis and multiple small pigmented lesions and confluent ulcerations in the gastric body and antrum. Pathology revealed poorly differentiated malignant neoplasm consistent with malignant melanoma. Patient’s family decided on hospice care in view of the poor prognosis.
Discussion: Malignant melanoma is the 5th most common cancer in the United States and is responsible for >90% of skin cancer mortality. The GI system is the most common site of melanoma metastases . The most commonly involved GI sites include small bowel, colon, rectum and less commonly stomach. Symptoms are not specific and includes anemia, abdominal pain, GI bleed among others. Diagnosis is suggested by cross sectional imaging and endoscopic examination. Three morphological types are described. The 1st type consists of melanotic nodules, often ulcerated at the tip. The 2nd type describes elevated submucosal masses with apical ulceration. The 3rd type defines masses with variable necrosis and melanosis. Pathological and immunohistochemical inspection confirms the diagnosis via immunostaining with S-100, Sox10, MART-1, HMB-45 and tyrosinase. Surgical resection can be curative in localized disease. In metastatic disease patients are referred to targeted therapy, immunotherapy and/or radiation therapy. Prognosis is poor if GI involvement with a median survival of < 1 year.

Figure: Panel 1, Figure A: Abdominal CT scan showed gastric irregularity, large ascites and abdominal masses concerning for peritoneal carcinomatosis; Figure B, C: Upper endoscopy showing severe gastritis and multiple small pigmented lesions and confluent ulcerations in the gastric body and antrum; Figure D, E, F: Hematoxylin and eosin stain, HMB45 and SOX10 immunohistochemistry respectively showing poorly differentiated malignant neoplasm consistent with malignant melanoma
Disclosures:
Maxim Kostyk indicated no relevant financial relationships.
Kevin Koch indicated no relevant financial relationships.
Fady G. Haddad indicated no relevant financial relationships.
Maxim Kostyk, DO1, Kevin Koch, DO1, Fady G. Haddad, MD2. P0640 - Malignant Melanoma Presenting With Upper Gastrointestinal Bleeding!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
