Sunday Poster Session
Category: GI Bleeding
P0644 - Bleeding Duodenal Varices: A Case Series
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Charles Yang, DO
Thomas Jefferson University
Voorhees, NJ
Presenting Author(s)
Charles Yang, DO1, Trinava Roy, DO1, Matthew Everwine, DO1, Christopher Chhoun, DO1, Nicholas Mason, DO1, Charles Snyder, MD2
1Thomas Jefferson University, Voorhees, NJ; 2Thomas Jefferson University, Camden, NJ
Introduction: Duodenal varices (DVs) are an infrequently reported phenomenon and encompass 0.4% of patients with portal hypertension. Cirrhosis is the most common hepatic cause of DVs and comprise 30% of all DVs cases. We describe two cases of duodenal varices that presented to the same hospital within a one-year period.
Case Description/Methods: Case 1 describes a 56-year-old male with history of daily alcohol use (six beers/day) that presented with hematochezia and hematemesis. Patient was not a known cirrhotic. Esophagogastroduodenoscopy (EGD) exhibited type 1 gastroesophageal varices (GOV type 1) and type 2 isolated gastric varices (IGV type 2). Examination of the duodenum revealed large, > 5 mm non-bleeding varices within the duodenal bulb and in the second portion of the duodenum. Push enteroscopy revealed red blood in the jejunum. No focal source was identified. Transjugular intrahepatic portosystemic shunt (TIPS) was well-tolerated. Pre-TIPS portosystemic gradient was 13 mmHg, post-TIPS portosystemic gradient was 5 mmHg. Case 2 describes a 62-year-old male with history of alcohol related cirrhosis presented after being found down. EGD demonstrated large, >5mm duodenal varices with white nipple and red center. One band was successfully placed. Type 2 gastroesophageal varices (GOV type 2) were also observed without bleeding. Patient was evaluated for TIPS, but was declined due to having heart failure with reduced ejection fraction.
Discussion: Duodenal varices are a rare entity related to portal hypertension. DVs are organized into two major subsets; hepatic (two thirds of cases) or extrahepatic (one third of cases), with cirrhosis being the most common hepatic cause. Other etiologies of DV such as superior mesenteric vein outflow obstruction, schistosomiasis and pancreatic malignancy have been reported. Due to the relative fragility of the duodenum, bleeds can be catastrophic and result in symptoms such as hematemesis, hematochezia or melena with a mortality of up to 40%. Diagnosis of DV is made during endoscopic evaluation. Other diagnostic modalities include barium studies, splenoportography, and other angiography. Due to the rarity of this disease, there are no current guidelines for management of non-bleeding DVs. Current treatment modalities vary from minimally invasive endoscopic therapy to surgical shunt creation. While there is a scarcity of information involving duodenal varices, these unique cases illustrate symptomatology and practical therapeutic considerations for this rare malady.

Disclosures:
Charles Yang, DO1, Trinava Roy, DO1, Matthew Everwine, DO1, Christopher Chhoun, DO1, Nicholas Mason, DO1, Charles Snyder, MD2. P0644 - Bleeding Duodenal Varices: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Thomas Jefferson University, Voorhees, NJ; 2Thomas Jefferson University, Camden, NJ
Introduction: Duodenal varices (DVs) are an infrequently reported phenomenon and encompass 0.4% of patients with portal hypertension. Cirrhosis is the most common hepatic cause of DVs and comprise 30% of all DVs cases. We describe two cases of duodenal varices that presented to the same hospital within a one-year period.
Case Description/Methods: Case 1 describes a 56-year-old male with history of daily alcohol use (six beers/day) that presented with hematochezia and hematemesis. Patient was not a known cirrhotic. Esophagogastroduodenoscopy (EGD) exhibited type 1 gastroesophageal varices (GOV type 1) and type 2 isolated gastric varices (IGV type 2). Examination of the duodenum revealed large, > 5 mm non-bleeding varices within the duodenal bulb and in the second portion of the duodenum. Push enteroscopy revealed red blood in the jejunum. No focal source was identified. Transjugular intrahepatic portosystemic shunt (TIPS) was well-tolerated. Pre-TIPS portosystemic gradient was 13 mmHg, post-TIPS portosystemic gradient was 5 mmHg. Case 2 describes a 62-year-old male with history of alcohol related cirrhosis presented after being found down. EGD demonstrated large, >5mm duodenal varices with white nipple and red center. One band was successfully placed. Type 2 gastroesophageal varices (GOV type 2) were also observed without bleeding. Patient was evaluated for TIPS, but was declined due to having heart failure with reduced ejection fraction.
Discussion: Duodenal varices are a rare entity related to portal hypertension. DVs are organized into two major subsets; hepatic (two thirds of cases) or extrahepatic (one third of cases), with cirrhosis being the most common hepatic cause. Other etiologies of DV such as superior mesenteric vein outflow obstruction, schistosomiasis and pancreatic malignancy have been reported. Due to the relative fragility of the duodenum, bleeds can be catastrophic and result in symptoms such as hematemesis, hematochezia or melena with a mortality of up to 40%. Diagnosis of DV is made during endoscopic evaluation. Other diagnostic modalities include barium studies, splenoportography, and other angiography. Due to the rarity of this disease, there are no current guidelines for management of non-bleeding DVs. Current treatment modalities vary from minimally invasive endoscopic therapy to surgical shunt creation. While there is a scarcity of information involving duodenal varices, these unique cases illustrate symptomatology and practical therapeutic considerations for this rare malady.

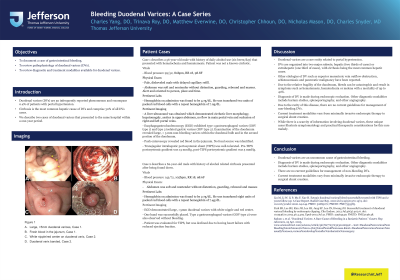
Figure: A. Large, >5mm duodenal varices, Case 1.
B. Fresh blood in the jejunum, Case 1.
C. White nipple/red center on duodenal varix, Case 2.
D. Duodenal varix banded, Case 2.
B. Fresh blood in the jejunum, Case 1.
C. White nipple/red center on duodenal varix, Case 2.
D. Duodenal varix banded, Case 2.
Disclosures:
Charles Yang indicated no relevant financial relationships.
Trinava Roy indicated no relevant financial relationships.
Matthew Everwine indicated no relevant financial relationships.
Christopher Chhoun indicated no relevant financial relationships.
Nicholas Mason indicated no relevant financial relationships.
Charles Snyder indicated no relevant financial relationships.
Charles Yang, DO1, Trinava Roy, DO1, Matthew Everwine, DO1, Christopher Chhoun, DO1, Nicholas Mason, DO1, Charles Snyder, MD2. P0644 - Bleeding Duodenal Varices: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
