Sunday Poster Session
Category: GI Bleeding
P0653 - Ethanolamine Oleate Treatment of Intestinal Phlebectasias
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- RT
Richard Trieu, MD
University of Arizona–Banner University Medical Center
Tucson, AZ
Presenting Author(s)
Richard Trieu, MD1, Joseph Kim, MD2, Shivanand Bomman, MD1, Cameron Thompson, MD3
1University of Arizona–Banner University Medical Center, Tucson, AZ; 2University of Arizona–Banner University Medical Center,, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ
Introduction: Phlebectasias are vascular abnormalities defined as small bowel tortuous venous dilations that are typically asymptomatic and incidentally found. We report the first case of symptomatic phlebectasia treated with ethanolamine oleate.
Case Description/Methods: A 69-year-old male has a history of gastric bypass, chronic kidney disease, and iron deficiency anemia. The patient had a watchman device placement 2-months ago complicated by anemia. Phlebectasias on endoscopic evaluation via push enteroscopy, and video capsule endoscopy. No active bleeding was found. Dual antiplatelet therapy was continued upon discharge 2 months prior. Over the past week, he had daily melena. On evaluation, the patient was tachycardic to 126, had a blood pressure of 95/60 mmHg, and had subconjunctival pallor. Labs revealed: 5.9 g/dL, MCV 93dL, Plt 275 K/uL, Pt 13.6, INR 1.2, aPtt 31.8 seconds, BUN: 38, Cr. 1.38 mg/dL.
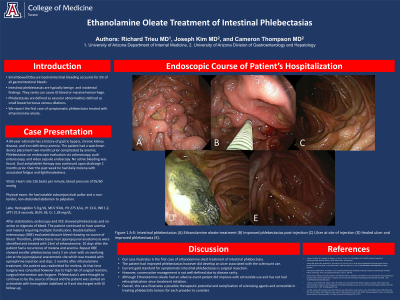
After stabilization, endoscopy and VCE showed phlebectasias and no active or stigmata of bleed. The patient continued to have anemia and melena requiring multiple transfusions. Double balloon enteroscopy (DBE) evaluated obscure bleed showing no source of the bleed. Phlebectasias near jejunojejunal anastomosis were thought to be the assumed source of blood loss and were treated with 13ml of ethanolamine. 10 days after, the patient developed melena and anemia. Repeat DBE showed smaller phlebectasias and a 2 cm ulcer with an overlying clot near the previous injection site which was treated with epinephrine injection and clips. 2 months after discharge the patient had a recurrence of melena. Repeat endoscopic evaluation was again only significant for phlebectasias. Therefore, phlebectasias were treated with subcutaneous octreotide and the patient has not had a recurrence of bleeding for 4 months.
Discussion: Intestinal phelbectasias conservative management is not well-defined due to disease rarity. This is the first case of Ethanolamine oleate-treated intestinal phlebectasia. Although he initially improved, his course was complicated by an ulcer. In the end, the patient had successful treatment with octreotide. This case illustrates possible therapeutic agents and complications in treating phlebectasias for providers to consider.

Disclosures:
Richard Trieu, MD1, Joseph Kim, MD2, Shivanand Bomman, MD1, Cameron Thompson, MD3. P0653 - Ethanolamine Oleate Treatment of Intestinal Phlebectasias, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona–Banner University Medical Center, Tucson, AZ; 2University of Arizona–Banner University Medical Center,, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ
Introduction: Phlebectasias are vascular abnormalities defined as small bowel tortuous venous dilations that are typically asymptomatic and incidentally found. We report the first case of symptomatic phlebectasia treated with ethanolamine oleate.
Case Description/Methods: A 69-year-old male has a history of gastric bypass, chronic kidney disease, and iron deficiency anemia. The patient had a watchman device placement 2-months ago complicated by anemia. Phlebectasias on endoscopic evaluation via push enteroscopy, and video capsule endoscopy. No active bleeding was found. Dual antiplatelet therapy was continued upon discharge 2 months prior. Over the past week, he had daily melena. On evaluation, the patient was tachycardic to 126, had a blood pressure of 95/60 mmHg, and had subconjunctival pallor. Labs revealed: 5.9 g/dL, MCV 93dL, Plt 275 K/uL, Pt 13.6, INR 1.2, aPtt 31.8 seconds, BUN: 38, Cr. 1.38 mg/dL.
After stabilization, endoscopy and VCE showed phlebectasias and no active or stigmata of bleed. The patient continued to have anemia and melena requiring multiple transfusions. Double balloon enteroscopy (DBE) evaluated obscure bleed showing no source of the bleed. Phlebectasias near jejunojejunal anastomosis were thought to be the assumed source of blood loss and were treated with 13ml of ethanolamine. 10 days after, the patient developed melena and anemia. Repeat DBE showed smaller phlebectasias and a 2 cm ulcer with an overlying clot near the previous injection site which was treated with epinephrine injection and clips. 2 months after discharge the patient had a recurrence of melena. Repeat endoscopic evaluation was again only significant for phlebectasias. Therefore, phlebectasias were treated with subcutaneous octreotide and the patient has not had a recurrence of bleeding for 4 months.
Discussion: Intestinal phelbectasias conservative management is not well-defined due to disease rarity. This is the first case of Ethanolamine oleate-treated intestinal phlebectasia. Although he initially improved, his course was complicated by an ulcer. In the end, the patient had successful treatment with octreotide. This case illustrates possible therapeutic agents and complications in treating phlebectasias for providers to consider.

Figure: Figure 1 A-F: Intestinal phlebectasias (A) Ethanolamine oleate treatment (B) Ulcer at the site of injection (C) Improved phlebectasias post-injection (D) Healed ulcer and improved phlebectasia(E).
Disclosures:
Richard Trieu indicated no relevant financial relationships.
Joseph Kim indicated no relevant financial relationships.
Shivanand Bomman indicated no relevant financial relationships.
Cameron Thompson indicated no relevant financial relationships.
Richard Trieu, MD1, Joseph Kim, MD2, Shivanand Bomman, MD1, Cameron Thompson, MD3. P0653 - Ethanolamine Oleate Treatment of Intestinal Phlebectasias, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
