Sunday Poster Session
Category: GI Bleeding
P0673 - Hemorrhagic Shock as an Unusual Presentation of Mallory Weiss Syndrome: A Case Report
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Chidiebele E. Omaliko, MD
One Brooklyn Health-Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Award: Presidential Poster Award
Chidiebele Omaliko, MD1, Swathi Rajagopal, MD1, Muhammad F. Ahmed, MD2, Chidiebube J. Ugwu, MD3, Elliot Bigajer, MD1
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3East Tennessee State University, Johnson City, TN
Introduction: Mallory-Weiss Syndrome (MWS) is a common cause of acute upper gastrointestinal bleeding due to mucosal lacerations in the distal esophagus and proximal stomach from forceful or prolonged vomiting or retching. We present a case of hemorrhagic shock as an unusual presentation of MWS and discuss the associated factors and management strategies.
Case Description/Methods: A 68-year-old female with ESRD on hemodialysis, heart failure, coronary artery disease (status post CABG and recent stent placement, on aspirin and clopidogrel), hypertension, COPD, Hepatitis C infection with HCC but no cirrhosis, status post TACE (in remission) and chronic thrombocytopenia, presented due to bloody vomiting during hemodialysis with 10 seconds of possible seizure and weakness. Vital signs were unstable with BP of 83/54mmHg. Examination showed a mildly tender abdomen with brown reddish tinted stool on digital rectal exam. Investigations were positive for a drop in Hb from a baseline of 12g/dl to 7.5 g/dl and a platelet count of 49,000/uL. After initial stabilization and transfusion, she had recurrent vomiting with massive hematemesis, hypotension and tachycardia requiring intubation, mechanical ventilation and multiple blood transfusions for drop in Hb to 6.1g/dl. Emergent esophagogastroduodenoscopy revealed an actively bleeding Mallory-Weiss tear in the distal esophagus, which was successfully controlled using endoscopic clips. No other source of bleeding was found, with no varices. She was managed with proton pump inhibitors, antibiotics, multiple blood transfusions, vasopressin and conjugated estrogens with improvement in clinical condition.
Discussion: MWS accounts for 5-15% of upper GI bleeding cases and lacerations are typically single, although two or three tears can occur. Lacerations in MWS often cause bleeding from submucosal arteries. Hematemesis is the most common presentation, but as seen in our patient, shock can occur but is rare. Only two cases of shock from MWS were found in the literature, one associated with binge drinking and the other with antiplatelet therapy and surgery. Our patient was on two antiplatelet agents and also had thrombocytopenia and ESRD requiring dialysis. Diagnosis of MWS is usually made through upper GI endoscopy, which allows visualization of the tears. Treatment options include endoscopy with clip placement, band ligation, or epinephrine injection at the bleeding site. MWS should be considered in cases of hemorrhagic shock.

Disclosures:
Chidiebele Omaliko, MD1, Swathi Rajagopal, MD1, Muhammad F. Ahmed, MD2, Chidiebube J. Ugwu, MD3, Elliot Bigajer, MD1. P0673 - Hemorrhagic Shock as an Unusual Presentation of Mallory Weiss Syndrome: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Chidiebele Omaliko, MD1, Swathi Rajagopal, MD1, Muhammad F. Ahmed, MD2, Chidiebube J. Ugwu, MD3, Elliot Bigajer, MD1
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3East Tennessee State University, Johnson City, TN
Introduction: Mallory-Weiss Syndrome (MWS) is a common cause of acute upper gastrointestinal bleeding due to mucosal lacerations in the distal esophagus and proximal stomach from forceful or prolonged vomiting or retching. We present a case of hemorrhagic shock as an unusual presentation of MWS and discuss the associated factors and management strategies.
Case Description/Methods: A 68-year-old female with ESRD on hemodialysis, heart failure, coronary artery disease (status post CABG and recent stent placement, on aspirin and clopidogrel), hypertension, COPD, Hepatitis C infection with HCC but no cirrhosis, status post TACE (in remission) and chronic thrombocytopenia, presented due to bloody vomiting during hemodialysis with 10 seconds of possible seizure and weakness. Vital signs were unstable with BP of 83/54mmHg. Examination showed a mildly tender abdomen with brown reddish tinted stool on digital rectal exam. Investigations were positive for a drop in Hb from a baseline of 12g/dl to 7.5 g/dl and a platelet count of 49,000/uL. After initial stabilization and transfusion, she had recurrent vomiting with massive hematemesis, hypotension and tachycardia requiring intubation, mechanical ventilation and multiple blood transfusions for drop in Hb to 6.1g/dl. Emergent esophagogastroduodenoscopy revealed an actively bleeding Mallory-Weiss tear in the distal esophagus, which was successfully controlled using endoscopic clips. No other source of bleeding was found, with no varices. She was managed with proton pump inhibitors, antibiotics, multiple blood transfusions, vasopressin and conjugated estrogens with improvement in clinical condition.
Discussion: MWS accounts for 5-15% of upper GI bleeding cases and lacerations are typically single, although two or three tears can occur. Lacerations in MWS often cause bleeding from submucosal arteries. Hematemesis is the most common presentation, but as seen in our patient, shock can occur but is rare. Only two cases of shock from MWS were found in the literature, one associated with binge drinking and the other with antiplatelet therapy and surgery. Our patient was on two antiplatelet agents and also had thrombocytopenia and ESRD requiring dialysis. Diagnosis of MWS is usually made through upper GI endoscopy, which allows visualization of the tears. Treatment options include endoscopy with clip placement, band ligation, or epinephrine injection at the bleeding site. MWS should be considered in cases of hemorrhagic shock.

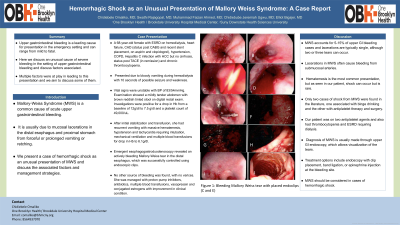
Figure: Image Depicting Mallory Weis Tear (A) with placed endoclips for Bleeding Control (C and E)
Disclosures:
Chidiebele Omaliko indicated no relevant financial relationships.
Swathi Rajagopal indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
Chidiebube Ugwu indicated no relevant financial relationships.
Elliot Bigajer indicated no relevant financial relationships.
Chidiebele Omaliko, MD1, Swathi Rajagopal, MD1, Muhammad F. Ahmed, MD2, Chidiebube J. Ugwu, MD3, Elliot Bigajer, MD1. P0673 - Hemorrhagic Shock as an Unusual Presentation of Mallory Weiss Syndrome: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

