Sunday Poster Session
Category: IBD
P0742 - Prevalence and Risk of Migraine in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Yashwitha Sai Pulakurthi, MBBS
New York Medical College-Saint Michael's Medical Center
Newark, New Jersey
Presenting Author(s)
Arankesh Mahadevan, MBBS1, Yashwitha Sai Pulakurthi, MBBS2, Rishabh Baskara Salian, MBBS3, Naga Vamsi Krishna Machineni, MBBS4, Sudhir Reddy. Pasham, MD5, Jayasree Ravilla, MD6, Prabhsimran Singh, MBBS7, Jahnavi Ethakota, MBBS8, Harshavardhan Polamarasetty, MBBS9, Rupak Desai, MBBS10
1SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India; 2New York Medical College-Saint Michael's Medical Center, Newark, NJ; 3Kasturba Medical College, Mangalore, Karnataka, India; 4Siddhartha Medical College, Cincinnati, OH; 5Guthrie Robert Packer Hospital, Sayre, PA; 6Monmouth Medical Center/RWJBH, Long Branch, NJ; 7Government Medical College, Amritsar, Punjab, India; 8Henry Ford Allegiance Health, Jackson, MI; 9Maharajah's Institute of Medical Sciences, Newark, Andhra Pradesh, India; 10Outcomes Research, Atlanta, GA
Introduction: Inflammatory bowel disease (IBD) is a complex autoimmune condition characterized by diverse risk factors and pathophysiologies. There is a hypothesized linkage between neurological and gastrointestinal disorders, possibly through the alterations in the "gut-brain axis". Migraines, defined as episodic neuroinflammatory conditions, are believed to have a potential association with systemic inflammation. However, the existing literature lacks comprehensive exploration of IBD as a potential risk factor for migraines. Our aim is to analyze the association between migraines and IBD through a systematic review and meta-analysis.
Methods: We conducted an extensive search of PubMed, Scopus, and Google Scholar until May 2023, screening for studies that reported the prevalence of migraines in IBD patients using MeSH and TiAB terms. In addition, we performed a cross-citation search. Our literature search yielded 117 reports. After pre-screening exclusion, 66 reports were eligible for screening. Binary random-effects models were used to perform meta-analysis. The I2 statistics was used to assess heterogeneity, and sensitivity analysis was done using the leave-one-out method.
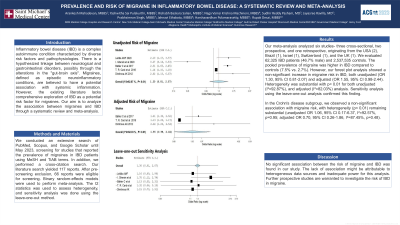
Results: Our meta-analysis analyzed six studies- three cross-sectional, two prospective, and one retrospective, originating from the USA (2), Brazil (1), Israel (1), Switzerland (1), and the UK (1). We evaluated 62,325 IBD patients (46.7% male) and 2,537,535 controls. The pooled prevalence of migraine was higher in IBD compared to controls (7.5% vs. 2.7%). However, our forest plot analysis showed a non-significant increase in migraine risk in IBD, both unadjusted (OR 1.30, 95% CI 0.81-2.07) and adjusted (OR 1.55, 95% CI 0.98-2.44). Heterogeneity was substantial with p< 0.01 for both unadjusted (I²=92.87%), and adjusted (I²=82.03%) analysis. Sensitivity analysis using the leave-one-out analysis confirmed this finding.
In the Crohn's disease subgroup, we observed a non-significant association with migraine risk, with heterogeneity (p< 0.01) remaining substantial (unadjusted OR 1.06, 95% CI 0.17-6.37, I²=92.57%, p=0.95; adjusted OR 0.70, 95% CI 0.26-1.86, I²=87.45%, p=0.48).
Discussion: No significant association between the risk of migraine and IBD was found in our study. The lack of association might be attributable to heterogeneous data sources and inadequate power for this analysis. Further prospective studies are warranted to investigate the risk of IBD in migraine.

Disclosures:
Arankesh Mahadevan, MBBS1, Yashwitha Sai Pulakurthi, MBBS2, Rishabh Baskara Salian, MBBS3, Naga Vamsi Krishna Machineni, MBBS4, Sudhir Reddy. Pasham, MD5, Jayasree Ravilla, MD6, Prabhsimran Singh, MBBS7, Jahnavi Ethakota, MBBS8, Harshavardhan Polamarasetty, MBBS9, Rupak Desai, MBBS10. P0742 - Prevalence and Risk of Migraine in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India; 2New York Medical College-Saint Michael's Medical Center, Newark, NJ; 3Kasturba Medical College, Mangalore, Karnataka, India; 4Siddhartha Medical College, Cincinnati, OH; 5Guthrie Robert Packer Hospital, Sayre, PA; 6Monmouth Medical Center/RWJBH, Long Branch, NJ; 7Government Medical College, Amritsar, Punjab, India; 8Henry Ford Allegiance Health, Jackson, MI; 9Maharajah's Institute of Medical Sciences, Newark, Andhra Pradesh, India; 10Outcomes Research, Atlanta, GA
Introduction: Inflammatory bowel disease (IBD) is a complex autoimmune condition characterized by diverse risk factors and pathophysiologies. There is a hypothesized linkage between neurological and gastrointestinal disorders, possibly through the alterations in the "gut-brain axis". Migraines, defined as episodic neuroinflammatory conditions, are believed to have a potential association with systemic inflammation. However, the existing literature lacks comprehensive exploration of IBD as a potential risk factor for migraines. Our aim is to analyze the association between migraines and IBD through a systematic review and meta-analysis.
Methods: We conducted an extensive search of PubMed, Scopus, and Google Scholar until May 2023, screening for studies that reported the prevalence of migraines in IBD patients using MeSH and TiAB terms. In addition, we performed a cross-citation search. Our literature search yielded 117 reports. After pre-screening exclusion, 66 reports were eligible for screening. Binary random-effects models were used to perform meta-analysis. The I2 statistics was used to assess heterogeneity, and sensitivity analysis was done using the leave-one-out method.
Results: Our meta-analysis analyzed six studies- three cross-sectional, two prospective, and one retrospective, originating from the USA (2), Brazil (1), Israel (1), Switzerland (1), and the UK (1). We evaluated 62,325 IBD patients (46.7% male) and 2,537,535 controls. The pooled prevalence of migraine was higher in IBD compared to controls (7.5% vs. 2.7%). However, our forest plot analysis showed a non-significant increase in migraine risk in IBD, both unadjusted (OR 1.30, 95% CI 0.81-2.07) and adjusted (OR 1.55, 95% CI 0.98-2.44). Heterogeneity was substantial with p< 0.01 for both unadjusted (I²=92.87%), and adjusted (I²=82.03%) analysis. Sensitivity analysis using the leave-one-out analysis confirmed this finding.
In the Crohn's disease subgroup, we observed a non-significant association with migraine risk, with heterogeneity (p< 0.01) remaining substantial (unadjusted OR 1.06, 95% CI 0.17-6.37, I²=92.57%, p=0.95; adjusted OR 0.70, 95% CI 0.26-1.86, I²=87.45%, p=0.48).
Discussion: No significant association between the risk of migraine and IBD was found in our study. The lack of association might be attributable to heterogeneous data sources and inadequate power for this analysis. Further prospective studies are warranted to investigate the risk of IBD in migraine.

Figure: Forest plot depicting unadjusted and adjusted odds ratios for risk of migraine in IBD
Disclosures:
Arankesh Mahadevan indicated no relevant financial relationships.
Yashwitha Sai Pulakurthi indicated no relevant financial relationships.
Rishabh Baskara Salian indicated no relevant financial relationships.
Naga Vamsi Krishna Machineni indicated no relevant financial relationships.
Sudhir Pasham indicated no relevant financial relationships.
Jayasree Ravilla indicated no relevant financial relationships.
Prabhsimran Singh indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Harshavardhan Polamarasetty indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Arankesh Mahadevan, MBBS1, Yashwitha Sai Pulakurthi, MBBS2, Rishabh Baskara Salian, MBBS3, Naga Vamsi Krishna Machineni, MBBS4, Sudhir Reddy. Pasham, MD5, Jayasree Ravilla, MD6, Prabhsimran Singh, MBBS7, Jahnavi Ethakota, MBBS8, Harshavardhan Polamarasetty, MBBS9, Rupak Desai, MBBS10. P0742 - Prevalence and Risk of Migraine in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
