Sunday Poster Session
Category: IBD
P0776 - The Impact of Health Insurance, Provider Status, and Biologic Use on Vaccination Documentation in Inflammatory Bowel Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Gabriel Heering, MD
Westchester Medical Center
New York, NY
Presenting Author(s)
Gabriel Heering, MD, Jakob Saidman, MD, Jessie Stephens, BS, Bessie Roca, BS, Elizabeth Drugge, MPH, PhD, Khalid Farhan, MPH, Meghan Work, MPH, PhD, Dana Berg, MD, Edward Lebovics, MD, FACG
Westchester Medical Center, Valhalla, NY
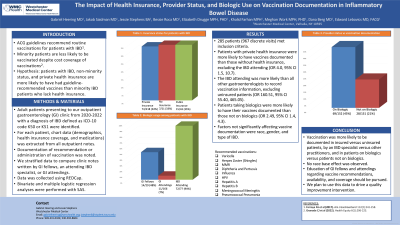
Introduction: ACG guidelines recommend routine vaccinations for patients with IBD. Minority patients are less likely to be vaccinated despite cost coverage of vaccinations. We hypothesized that patients with IBD, non-minority status, and private health insurance are more likely to have had guideline-recommended vaccines than minority IBD patients who lack health insurance.
Methods: Adult patients presenting to our outpatient gastroenterology (GI) clinic from 2020-2022 with a diagnosis of IBD defined as ICD-10 code K50 or K51 were identified. For each patient, chart data (demographics, health insurance coverage, and medications) was extracted from all outpatient notes. Documentation of recommendation or administration of vaccination was noted. We stratified data to compare clinic notes written by GI fellows, an attending IBD specialist, or GI attendings. Data was collected using REDCap. Bivariate and multiple logistic regression analyses were performed with SAS.
Results: 285 patients (967 discrete visits) met inclusion criteria. Vaccines were documented by insurance status: private insurance 74/218 (34%), public insurance 15/43 (35%), and no insurance 7/21 (33%); by provider status: GI fellows 14/29 (48%), GI attendings 11/166 (7%), and an IBD attending 72/77 (94%); by biologic use: on biologic 69/152 (45%), not on biologic 28/131 (21%). Patients with private health insurance were more likely to have vaccines documented than those without health insurance, excluding the IBD attending (OR 4.0, 95% CI 1.5, 10.7). The IBD attending was more likely than all other gastroenterologists to record vaccination information, excluding uninsured patients (OR 160.51, 95% CI 55.40, 465.05). Patients taking biologics were more likely to have their vaccines documented than those not on biologics (OR 2.49, 95% CI 1.4, 4.3). Factors not significantly affecting vaccine documentation were race, gender, and type of IBD.
Discussion: Vaccination was more likely to be documented in insured versus uninsured patients, by an IBD specialist versus other practitioners, and in patients on biologics versus patients not on biologics. No race base effect was observed. Education of GI fellows and attendings regarding vaccine recommendations, availability, and coverage should be pursued. We plan to use this data to drive a quality improvement intervention.
Disclosures:
Gabriel Heering, MD, Jakob Saidman, MD, Jessie Stephens, BS, Bessie Roca, BS, Elizabeth Drugge, MPH, PhD, Khalid Farhan, MPH, Meghan Work, MPH, PhD, Dana Berg, MD, Edward Lebovics, MD, FACG. P0776 - The Impact of Health Insurance, Provider Status, and Biologic Use on Vaccination Documentation in Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: ACG guidelines recommend routine vaccinations for patients with IBD. Minority patients are less likely to be vaccinated despite cost coverage of vaccinations. We hypothesized that patients with IBD, non-minority status, and private health insurance are more likely to have had guideline-recommended vaccines than minority IBD patients who lack health insurance.
Methods: Adult patients presenting to our outpatient gastroenterology (GI) clinic from 2020-2022 with a diagnosis of IBD defined as ICD-10 code K50 or K51 were identified. For each patient, chart data (demographics, health insurance coverage, and medications) was extracted from all outpatient notes. Documentation of recommendation or administration of vaccination was noted. We stratified data to compare clinic notes written by GI fellows, an attending IBD specialist, or GI attendings. Data was collected using REDCap. Bivariate and multiple logistic regression analyses were performed with SAS.
Results: 285 patients (967 discrete visits) met inclusion criteria. Vaccines were documented by insurance status: private insurance 74/218 (34%), public insurance 15/43 (35%), and no insurance 7/21 (33%); by provider status: GI fellows 14/29 (48%), GI attendings 11/166 (7%), and an IBD attending 72/77 (94%); by biologic use: on biologic 69/152 (45%), not on biologic 28/131 (21%). Patients with private health insurance were more likely to have vaccines documented than those without health insurance, excluding the IBD attending (OR 4.0, 95% CI 1.5, 10.7). The IBD attending was more likely than all other gastroenterologists to record vaccination information, excluding uninsured patients (OR 160.51, 95% CI 55.40, 465.05). Patients taking biologics were more likely to have their vaccines documented than those not on biologics (OR 2.49, 95% CI 1.4, 4.3). Factors not significantly affecting vaccine documentation were race, gender, and type of IBD.
Discussion: Vaccination was more likely to be documented in insured versus uninsured patients, by an IBD specialist versus other practitioners, and in patients on biologics versus patients not on biologics. No race base effect was observed. Education of GI fellows and attendings regarding vaccine recommendations, availability, and coverage should be pursued. We plan to use this data to drive a quality improvement intervention.
Disclosures:
Gabriel Heering indicated no relevant financial relationships.
Jakob Saidman indicated no relevant financial relationships.
Jessie Stephens indicated no relevant financial relationships.
Bessie Roca indicated no relevant financial relationships.
Elizabeth Drugge indicated no relevant financial relationships.
Khalid Farhan indicated no relevant financial relationships.
Meghan Work indicated no relevant financial relationships.
Dana Berg indicated no relevant financial relationships.
Edward Lebovics indicated no relevant financial relationships.
Gabriel Heering, MD, Jakob Saidman, MD, Jessie Stephens, BS, Bessie Roca, BS, Elizabeth Drugge, MPH, PhD, Khalid Farhan, MPH, Meghan Work, MPH, PhD, Dana Berg, MD, Edward Lebovics, MD, FACG. P0776 - The Impact of Health Insurance, Provider Status, and Biologic Use on Vaccination Documentation in Inflammatory Bowel Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
