Sunday Poster Session
Category: Interventional Endoscopy
P0856 - Sex Disparities in Diagnostic Workup Prior to ERCP: A Multicenter Retrospective Cohort Study
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Sarah Dwyer Holland, MD, MS
Brown University
Providence, RI
Presenting Author(s)
Sarah Dwyer Holland, MD, MS1, Garrett Weskamp, MD2, Gabriel Brutico, MD, MBS3, Ford Holland, MS4, David L. Diehl, MD5, Shaffer Mok, MD, MBS6
1Brown University, Providence, RI; 2University of Colorado, Aurora, CO; 3Saint Luke’s University Hospital, Bethlehem, PA; 4Independent Researcher, Providence, RI; 5Geisinger Medical Center, Danville, PA; 6Moffitt Cancer Center, Tampa, FL
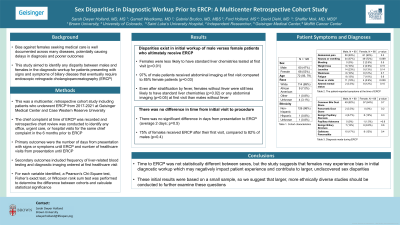
Introduction: Bias against females seeking medical care is well documented across many diseases. This bias can potentially cause significant delays in diagnosis and poorer outcomes. However, it is unknown whether a similar disparity among females is seen for diagnostic workup of biliary diseases that eventually require endoscopic retrograde cholangiopancreatography (ERCP). In this study we sought to determine diagnostic work-up disparities in female patients who eventually underwent ERCP.
Methods: We conducted a multi-center retrospective cohort study of patients who underwent ERCP at three tertiary care centers in the United States from December 2020 to December 2021. We assessed differences between males and females in the number of visits, number of days from presentation to ERCP, chief complaint, diagnosis, and laboratory and imaging workup at first visit using Pearson’s Chi-squared, Wilcoxon rank sum, and Fisher’s exact tests.
Results: A total of 68 female and 60 male patients were identified from chart review. Eighteen percent of males presented at their first encounter with fever or chills versus 6% of females (p= 0.03), but there were otherwise no differences in chief complaints between sexes. There was no difference in the number of males and females who were diagnosed with choledocholithiasis (p=0.7).
Eighteen percent of males and 25% of females had more than one visit before ERCP (p=0.4), and there was no difference between sexes in days from presentation until ERCP (p=0.5). There was a significant difference in the initial labs and imaging evaluation. Males received standard liver chemistries at 98% of initial visits compared to 85% in females (p=0.01). Males also had abdominal imaging ordered at 97% of initial visits compared to 85% for females (p=0.03). After excluding patients with fever, males remained more likely to have lab evaluation (p=0.01) and imaging evaluation (p=0.05) at initial visit.
Discussion: Although time to ERCP was not statistically different between sexes, the study results suggest that females may be experiencing bias in initial diagnostic workup, which may negatively impact patient experience and contribute to larger, undiscovered sex disparities in care for patients with biliary pathologies. Notably, these initial results were based on a small sample and we would suggest larger studies be conducted to further examine these questions.
Disclosures:
Sarah Dwyer Holland, MD, MS1, Garrett Weskamp, MD2, Gabriel Brutico, MD, MBS3, Ford Holland, MS4, David L. Diehl, MD5, Shaffer Mok, MD, MBS6. P0856 - Sex Disparities in Diagnostic Workup Prior to ERCP: A Multicenter Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brown University, Providence, RI; 2University of Colorado, Aurora, CO; 3Saint Luke’s University Hospital, Bethlehem, PA; 4Independent Researcher, Providence, RI; 5Geisinger Medical Center, Danville, PA; 6Moffitt Cancer Center, Tampa, FL
Introduction: Bias against females seeking medical care is well documented across many diseases. This bias can potentially cause significant delays in diagnosis and poorer outcomes. However, it is unknown whether a similar disparity among females is seen for diagnostic workup of biliary diseases that eventually require endoscopic retrograde cholangiopancreatography (ERCP). In this study we sought to determine diagnostic work-up disparities in female patients who eventually underwent ERCP.
Methods: We conducted a multi-center retrospective cohort study of patients who underwent ERCP at three tertiary care centers in the United States from December 2020 to December 2021. We assessed differences between males and females in the number of visits, number of days from presentation to ERCP, chief complaint, diagnosis, and laboratory and imaging workup at first visit using Pearson’s Chi-squared, Wilcoxon rank sum, and Fisher’s exact tests.
Results: A total of 68 female and 60 male patients were identified from chart review. Eighteen percent of males presented at their first encounter with fever or chills versus 6% of females (p= 0.03), but there were otherwise no differences in chief complaints between sexes. There was no difference in the number of males and females who were diagnosed with choledocholithiasis (p=0.7).
Eighteen percent of males and 25% of females had more than one visit before ERCP (p=0.4), and there was no difference between sexes in days from presentation until ERCP (p=0.5). There was a significant difference in the initial labs and imaging evaluation. Males received standard liver chemistries at 98% of initial visits compared to 85% in females (p=0.01). Males also had abdominal imaging ordered at 97% of initial visits compared to 85% for females (p=0.03). After excluding patients with fever, males remained more likely to have lab evaluation (p=0.01) and imaging evaluation (p=0.05) at initial visit.
Discussion: Although time to ERCP was not statistically different between sexes, the study results suggest that females may be experiencing bias in initial diagnostic workup, which may negatively impact patient experience and contribute to larger, undiscovered sex disparities in care for patients with biliary pathologies. Notably, these initial results were based on a small sample and we would suggest larger studies be conducted to further examine these questions.
Disclosures:
Sarah Dwyer Holland indicated no relevant financial relationships.
Garrett Weskamp indicated no relevant financial relationships.
Gabriel Brutico indicated no relevant financial relationships.
Ford Holland indicated no relevant financial relationships.
David Diehl: Boston Scientific – Consultant. Castle – Consultant. Laborie – Consultant. Merit Endotek – Consultant. Microtech – Consultant. Olympus – Consultant. OnePass Medical – Consultant. Pentax – Consultant. Steris – Consultant.
Shaffer Mok: Conmed – Consultant. Steris – Consultant.
Sarah Dwyer Holland, MD, MS1, Garrett Weskamp, MD2, Gabriel Brutico, MD, MBS3, Ford Holland, MS4, David L. Diehl, MD5, Shaffer Mok, MD, MBS6. P0856 - Sex Disparities in Diagnostic Workup Prior to ERCP: A Multicenter Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
