Sunday Poster Session
Category: Interventional Endoscopy
P0878 - Is There a Role of EUS in the “Watch-and-Wait” Strategy for Locally Advanced Rectal Cancer
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Bhargav Kansara, BS
USF Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Bhargav Kansara, BS1, Luis R.. Pena, MD, FACG2, Shaffer R. S.. Mok, MD2, Mark Friedman, MD2, Anjuli K.. Luthra, MD2, Aamir Dam, MD2
1USF Morsani College of Medicine, Tampa, FL; 2Moffitt Cancer Center, Tampa, FL
Introduction: Neoadjuvant chemoradiotherapy followed by surgery has been adopted as the standard of care for locally advanced rectal cancer (LARC). More recently, a nonoperative “watch-and-wait” strategy (WW) has been proposed to focus on organ preservation and reduce morbidity. The single necessary requirement to be eligible for WW is complete clinical response (cCR) following neoadjuvant treatment. The ideal endoscopic finding to support cCR is a white flat scar and no ulcerations nor fibrin. The presence of ulcers or mucosal irregularities should be considered suspicious for an incomplete response. Endoscopic mucosal biopsies have a low negative predictive value and can mislead both patients and surgeons into a WW strategy.
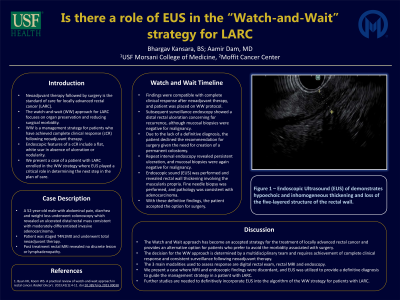
Case Description/Methods: Our patient is a 52-year-old male who initially presented with abdominal pain, weight loss and diarrhea. Colonoscopy revealed an ulcerated mass in the distal rectum, and biopsies were consistent with a moderately differentiated invasive adenocarcinoma. The patient was staged T4N1M0 and underwent total neoadjuvant therapy (TNT). Post treatment rectal MRI revealed no discrete lesion or lymphadenopathy, and findings were compatible with complete radiologic response. After multidisciplinary discussion, a WW approach was pursued. Subsequent surveillance endoscopy revealed a distal rectal ulceration, although mucosal biopsies were negative for malignancy. Based on the suspicous findings, the option of a permanent colostomy was presented, although the patient declined surgery given the lack of a definitive diagnosis. Repeat interval endoscopy revealed persistent ulceration, although mucosal biopsies were again negative. Endoscopic ultrasound (EUS) was pursued and revealed localized wall thickening in the rectal wall involving the muscularis propria (Figure 1). Fine needle biopsy was performed, and final pathology was consistent with adenocarcinoma. Given these definitive findings, the patient accepted the option of surgery.
Discussion: The negative impact of rectal surgery on quality of life is well known. The WW strategy has become an accepted approach and can provide patients an alternative option for the treatment of LARC. Central to the WW strategy is the achievement of cCR based on clinical exam, flexible endoscopy and high-resolution MRI. In this case, the MRI and endoscopic findings were discordant, and EUS provided definitive evidence of residual disease. Although further studies are needed, EUS may serve as an adjunct in the WW protocol.

Disclosures:
Bhargav Kansara, BS1, Luis R.. Pena, MD, FACG2, Shaffer R. S.. Mok, MD2, Mark Friedman, MD2, Anjuli K.. Luthra, MD2, Aamir Dam, MD2. P0878 - Is There a Role of EUS in the “Watch-and-Wait” Strategy for Locally Advanced Rectal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1USF Morsani College of Medicine, Tampa, FL; 2Moffitt Cancer Center, Tampa, FL
Introduction: Neoadjuvant chemoradiotherapy followed by surgery has been adopted as the standard of care for locally advanced rectal cancer (LARC). More recently, a nonoperative “watch-and-wait” strategy (WW) has been proposed to focus on organ preservation and reduce morbidity. The single necessary requirement to be eligible for WW is complete clinical response (cCR) following neoadjuvant treatment. The ideal endoscopic finding to support cCR is a white flat scar and no ulcerations nor fibrin. The presence of ulcers or mucosal irregularities should be considered suspicious for an incomplete response. Endoscopic mucosal biopsies have a low negative predictive value and can mislead both patients and surgeons into a WW strategy.
Case Description/Methods: Our patient is a 52-year-old male who initially presented with abdominal pain, weight loss and diarrhea. Colonoscopy revealed an ulcerated mass in the distal rectum, and biopsies were consistent with a moderately differentiated invasive adenocarcinoma. The patient was staged T4N1M0 and underwent total neoadjuvant therapy (TNT). Post treatment rectal MRI revealed no discrete lesion or lymphadenopathy, and findings were compatible with complete radiologic response. After multidisciplinary discussion, a WW approach was pursued. Subsequent surveillance endoscopy revealed a distal rectal ulceration, although mucosal biopsies were negative for malignancy. Based on the suspicous findings, the option of a permanent colostomy was presented, although the patient declined surgery given the lack of a definitive diagnosis. Repeat interval endoscopy revealed persistent ulceration, although mucosal biopsies were again negative. Endoscopic ultrasound (EUS) was pursued and revealed localized wall thickening in the rectal wall involving the muscularis propria (Figure 1). Fine needle biopsy was performed, and final pathology was consistent with adenocarcinoma. Given these definitive findings, the patient accepted the option of surgery.
Discussion: The negative impact of rectal surgery on quality of life is well known. The WW strategy has become an accepted approach and can provide patients an alternative option for the treatment of LARC. Central to the WW strategy is the achievement of cCR based on clinical exam, flexible endoscopy and high-resolution MRI. In this case, the MRI and endoscopic findings were discordant, and EUS provided definitive evidence of residual disease. Although further studies are needed, EUS may serve as an adjunct in the WW protocol.

Figure: Figure 1: EUS of the rectal wall.
Disclosures:
Bhargav Kansara indicated no relevant financial relationships.
Luis Pena indicated no relevant financial relationships.
Shaffer Mok: Conmed – Consultant. Steris – Consultant.
Mark Friedman indicated no relevant financial relationships.
Anjuli Luthra: Boston Scientific – Consultant.
Aamir Dam indicated no relevant financial relationships.
Bhargav Kansara, BS1, Luis R.. Pena, MD, FACG2, Shaffer R. S.. Mok, MD2, Mark Friedman, MD2, Anjuli K.. Luthra, MD2, Aamir Dam, MD2. P0878 - Is There a Role of EUS in the “Watch-and-Wait” Strategy for Locally Advanced Rectal Cancer, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
