Sunday Poster Session
Category: Liver
P0938 - Differences in Patient Characteristics and Outcomes by Hospital Size for Patients With Chronic Liver Disease and Acute Kidney Injury or Hepatorenal Syndrome
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Robert J. Wong, MD, MS, FACG
Stanford/VA Palo Alto
Palo Alto, CA
Presenting Author(s)
Robert J.. Wong, MD, MS, FACG1, Khurram Jamil, MD2, Kyle Hayes, MS3, Mohammed Fahim, MS4, Xingyue Huang, PhD5
1Stanford/VA Palo Alto, Palo Alto, CA; 2Mallinckrodt Pharmaceuticals, Bridgewater, NJ; 3Mallinckrodt Pharmaceuticals, St. Louis, MO; 4Mallinckrodt Pharmaceuticals, Plainsboro, NJ; 5Mallinckrodt Pharmaceuticals, Basking Ridge, NJ
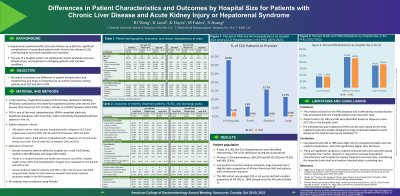
Introduction: Hepatorenal syndrome (HRS) and acute kidney injury (AKI) are significant complications in hospitalized patients with chronic liver disease (CLD), contributing to increased morbidity and mortality. The size of a hospital system can significantly impact available resources, infrastructure, and expertise in managing patients with complex conditions. We aimed to evaluate the impact of hospital size on patient outcomes among patients with CLD and AKI or HRS.
Methods: Hospitalized patients with CLD (including cirrhosis) from 2016 to 2022 were identified using the Premier Healthcare Database, one of the most comprehensive healthcare databases inclusive of over 1,041 hospitals/health systems in the US. Patients with CLD and AKI or HRS were identified by ICD-10-CM codes. Patients in the CLD+HRS cohort includes HRS+AKI patients. Overall outcomes were stratified by hospital size: small (< 100 beds), medium (100-499 beds), and large (500+ beds).
Results: A total of 2,991,056 hospitalized CLD patients were identified, representing 7.9% of all admissions during the study period. Of those CLD patients, 985,255 had AKI (32.9%) and 70,955 had HRS (2.4%). Compared to small and medium hospitals, large hospitals had a slightly higher proportion of African Americans (AA) and patients with commercial insurance. The HRS cohort was younger (63 vs. 59 years) and had a smaller proportion of AA (9% vs. 16%) compared to the AKI cohort. Overall in-hospital mortality in the HRS cohort was 47%, with slightly lower rate in the small, compared to medium and large hospitals (45% vs. 48% vs. 47%, respectively). A similar trend was observed for the AKI cohort, with small hospitals having lower mortality rate than medium and large hospitals (23% vs. 27% vs. 29%). Compared to AKI, the HRS cohort had higher rates of comorbidities, with the most significant being hepatic failure (40% vs. 10%), alcoholic cirrhosis (54% vs. 11%), alcoholic hepatic failure (19% vs. 2%), portal hypertension (47% vs. 9%), and esophageal varices (27% vs. 5%).
Discussion: CLD patients with AKI or HRS had a high risk of in-hospital mortality and CLD-related complications, with HRS significantly higher than AKI alone. There are significant variations in patient characteristics and outcomes based on hospital size. Further research is required to evaluate how patient characteristics and hospital size impact treatment and outcomes, considering the important role small and medium hospitals play in providing care.
Disclosures:
Robert J.. Wong, MD, MS, FACG1, Khurram Jamil, MD2, Kyle Hayes, MS3, Mohammed Fahim, MS4, Xingyue Huang, PhD5. P0938 - Differences in Patient Characteristics and Outcomes by Hospital Size for Patients With Chronic Liver Disease and Acute Kidney Injury or Hepatorenal Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Stanford/VA Palo Alto, Palo Alto, CA; 2Mallinckrodt Pharmaceuticals, Bridgewater, NJ; 3Mallinckrodt Pharmaceuticals, St. Louis, MO; 4Mallinckrodt Pharmaceuticals, Plainsboro, NJ; 5Mallinckrodt Pharmaceuticals, Basking Ridge, NJ
Introduction: Hepatorenal syndrome (HRS) and acute kidney injury (AKI) are significant complications in hospitalized patients with chronic liver disease (CLD), contributing to increased morbidity and mortality. The size of a hospital system can significantly impact available resources, infrastructure, and expertise in managing patients with complex conditions. We aimed to evaluate the impact of hospital size on patient outcomes among patients with CLD and AKI or HRS.
Methods: Hospitalized patients with CLD (including cirrhosis) from 2016 to 2022 were identified using the Premier Healthcare Database, one of the most comprehensive healthcare databases inclusive of over 1,041 hospitals/health systems in the US. Patients with CLD and AKI or HRS were identified by ICD-10-CM codes. Patients in the CLD+HRS cohort includes HRS+AKI patients. Overall outcomes were stratified by hospital size: small (< 100 beds), medium (100-499 beds), and large (500+ beds).
Results: A total of 2,991,056 hospitalized CLD patients were identified, representing 7.9% of all admissions during the study period. Of those CLD patients, 985,255 had AKI (32.9%) and 70,955 had HRS (2.4%). Compared to small and medium hospitals, large hospitals had a slightly higher proportion of African Americans (AA) and patients with commercial insurance. The HRS cohort was younger (63 vs. 59 years) and had a smaller proportion of AA (9% vs. 16%) compared to the AKI cohort. Overall in-hospital mortality in the HRS cohort was 47%, with slightly lower rate in the small, compared to medium and large hospitals (45% vs. 48% vs. 47%, respectively). A similar trend was observed for the AKI cohort, with small hospitals having lower mortality rate than medium and large hospitals (23% vs. 27% vs. 29%). Compared to AKI, the HRS cohort had higher rates of comorbidities, with the most significant being hepatic failure (40% vs. 10%), alcoholic cirrhosis (54% vs. 11%), alcoholic hepatic failure (19% vs. 2%), portal hypertension (47% vs. 9%), and esophageal varices (27% vs. 5%).
Discussion: CLD patients with AKI or HRS had a high risk of in-hospital mortality and CLD-related complications, with HRS significantly higher than AKI alone. There are significant variations in patient characteristics and outcomes based on hospital size. Further research is required to evaluate how patient characteristics and hospital size impact treatment and outcomes, considering the important role small and medium hospitals play in providing care.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table: Baseline Characteristics and Outcomes for CLD with AKI and CLD with HRS Cohorts
Disclosures:
Robert Wong: Exact Sciences – Grant/Research Support. Gilead Sciences – Consultant, Grant/Research Support. Thera Technologies – Grant/Research Support.
Khurram Jamil: Mallinckrodt Pharmaceuticals – Employee.
Kyle Hayes: Mallinckrodt Pharmaceuticals – Employee.
Mohammed Fahim: KMK consulting Inc. – Employee.
Xingyue Huang: Mallinckrodt Pharmaceuticals – Employee.
Robert J.. Wong, MD, MS, FACG1, Khurram Jamil, MD2, Kyle Hayes, MS3, Mohammed Fahim, MS4, Xingyue Huang, PhD5. P0938 - Differences in Patient Characteristics and Outcomes by Hospital Size for Patients With Chronic Liver Disease and Acute Kidney Injury or Hepatorenal Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
