Sunday Poster Session
Category: Liver
P1060 - When Corticosteroids Are Not Sufficient in Immune-Related Hepatitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DP
Deevyashali Parekh, MBBS
Houston Methodist Hospital
Houston, Texas
Presenting Author(s)
Ayushi Shah, MBBS1, Deevyashali Parekh, MBBS2, Shefali P. Mody, MBBS3, Mukul Divatia, MD2, Sudha Kodali, MD, MPH2
1Houston Methodist, Houston, TX; 2Houston Methodist Hospital, Houston, TX; 3Lokmanya Tilak Municipal Medical College, Mumbai, Maharashtra, India
Introduction: The response of various cancers to immunotherapy has led to increased use of immune check point inhibitors with need for increased knowledge about the side effects and management. We present a case of immune- related hepatitis (irH) that was steroid-refractory and discuss management.
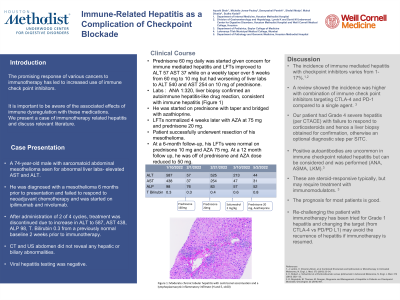
Case Description/Methods: 74-year-old male with sarcomatoid abdominal mesothelioma presented to the Hepatology clinic for elevated liver enzymes. After failure of response to neoadjuvant chemotherapy for his unresectable sarcoma, he has been started on ipilimumab and nivolumab. After 2 of 4 cycles, combination immunotherapy was discontinued due to increase in ALT to 587, AST 438, ALP 98, T. Bilirubin 0.3 from a previously normal baseline liver test. CT and US abdomen did not reveal any biliary abnormalities. Viral hepatitis testing was negative. No other new medications had been started. He was started on prednisone 60 mg daily. His liver enzymes improved initially but he did not tolerate a taper and had recurrent elevation with ALT 540 and AST 254. He was admitted for IV methylprednisolone at 2 mg/kg daily. Over a course of 4 weeks after this, he continued to need at least 60 mg prednisone and any taper was associated with an increase in liver enzymes. Labs showed ANA positive at 1:320. Liver biopsy was obtained, which showed a lymphoplasmacytic infiltration with centrizonal accentuation confirming irH. He was started on Azathioprine (AZA) and prednisone was continued. Liver enzymes completely normalized 4 weeks later with AZA at 75 mg and prednisone dose was tapered.
Discussion: Treatment of irH entails discontinuation of the offending agent if the severity is CTCAE 2 or higher until complete and consistent resolution is visible clinically and on laboratory investigations. Glucocorticoids should be initiated for Grade 2 and higher injury.
According to AASLD guidelines, prednisone or methylprednisolone if hospitalized, at 1-2 mg/kg daily in adults, or a lower dose of prednisone, 0.5 mg/kg mg daily for CTCAE 2 injury, should be initiated with taper over 4-6 weeks. If steroid refractory or no improvement in liver enzymes is seen in 3 days, evaluate TPMT status, and consider mycophenolate or AZA as in our patient. In our case, our patient had Grade 3 severe hepatitis with failure to respond to corticosteroids. This decreased the threshold for obtaining a liver biopsy, which is recommended for steroid-refractory disease, Grade 3 or higher hepatitis or if suspicion is present for DILI or AIH.

Disclosures:
Ayushi Shah, MBBS1, Deevyashali Parekh, MBBS2, Shefali P. Mody, MBBS3, Mukul Divatia, MD2, Sudha Kodali, MD, MPH2. P1060 - When Corticosteroids Are Not Sufficient in Immune-Related Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Houston Methodist, Houston, TX; 2Houston Methodist Hospital, Houston, TX; 3Lokmanya Tilak Municipal Medical College, Mumbai, Maharashtra, India
Introduction: The response of various cancers to immunotherapy has led to increased use of immune check point inhibitors with need for increased knowledge about the side effects and management. We present a case of immune- related hepatitis (irH) that was steroid-refractory and discuss management.
Case Description/Methods: 74-year-old male with sarcomatoid abdominal mesothelioma presented to the Hepatology clinic for elevated liver enzymes. After failure of response to neoadjuvant chemotherapy for his unresectable sarcoma, he has been started on ipilimumab and nivolumab. After 2 of 4 cycles, combination immunotherapy was discontinued due to increase in ALT to 587, AST 438, ALP 98, T. Bilirubin 0.3 from a previously normal baseline liver test. CT and US abdomen did not reveal any biliary abnormalities. Viral hepatitis testing was negative. No other new medications had been started. He was started on prednisone 60 mg daily. His liver enzymes improved initially but he did not tolerate a taper and had recurrent elevation with ALT 540 and AST 254. He was admitted for IV methylprednisolone at 2 mg/kg daily. Over a course of 4 weeks after this, he continued to need at least 60 mg prednisone and any taper was associated with an increase in liver enzymes. Labs showed ANA positive at 1:320. Liver biopsy was obtained, which showed a lymphoplasmacytic infiltration with centrizonal accentuation confirming irH. He was started on Azathioprine (AZA) and prednisone was continued. Liver enzymes completely normalized 4 weeks later with AZA at 75 mg and prednisone dose was tapered.
Discussion: Treatment of irH entails discontinuation of the offending agent if the severity is CTCAE 2 or higher until complete and consistent resolution is visible clinically and on laboratory investigations. Glucocorticoids should be initiated for Grade 2 and higher injury.
According to AASLD guidelines, prednisone or methylprednisolone if hospitalized, at 1-2 mg/kg daily in adults, or a lower dose of prednisone, 0.5 mg/kg mg daily for CTCAE 2 injury, should be initiated with taper over 4-6 weeks. If steroid refractory or no improvement in liver enzymes is seen in 3 days, evaluate TPMT status, and consider mycophenolate or AZA as in our patient. In our case, our patient had Grade 3 severe hepatitis with failure to respond to corticosteroids. This decreased the threshold for obtaining a liver biopsy, which is recommended for steroid-refractory disease, Grade 3 or higher hepatitis or if suspicion is present for DILI or AIH.

Figure: Moderate chronic lobular hepatitis with centrizonal accentuation and a lymphoplasmacytic inflammatory infiltrate (H and E, x100)
Disclosures:
Ayushi Shah indicated no relevant financial relationships.
Deevyashali Parekh indicated no relevant financial relationships.
Shefali Mody indicated no relevant financial relationships.
Mukul Divatia indicated no relevant financial relationships.
Sudha Kodali indicated no relevant financial relationships.
Ayushi Shah, MBBS1, Deevyashali Parekh, MBBS2, Shefali P. Mody, MBBS3, Mukul Divatia, MD2, Sudha Kodali, MD, MPH2. P1060 - When Corticosteroids Are Not Sufficient in Immune-Related Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
