Sunday Poster Session
Category: Liver
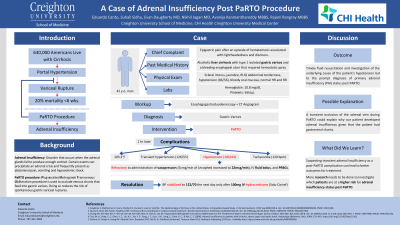
P1093 - A Case of Adrenal Insufficiency Post PaRTO Procedure
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Eduardo A. Canto, BS
Creighton University School of Medicine
Omaha, NE
Presenting Author(s)
Eduardo A. Canto, BS1, Suhail Sidhu, BS1, Evan Daugherty, MD2, Nikhil Jagan, MBBS2, Avanija Kanmanthareddy, MBBS2, Rajani Rangray, MBBS2
1Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: 630,000 adults in the United States live with cirrhosis. Variceal rupture is the deadliest complication from cirrhosis with a 20% mortality within six weeks after onset of hemorrhage. To manage portal hypertension secondary to chronic liver disease and prevent gastric varix rupture, plug-assisted retrograde transvenous obliteration (PaRTO) may be performed. Our case is the second of its kind to demonstrate transient adrenal insufficiency, a rare but life threatening complication, status post PaRTO.
Case Description/Methods: A 42 year-old man with past medical history of alcoholic liver cirrhosis with type I isolated gastric varices and a bleeding esophageal ulcer that required hemostatic spray presented with complaints of epigastric pain after an episode of hematemesis associated with lightheadedness and dizziness. Physical exam revealed scleral icterus, jaundice, RUQ abdominal tenderness, hypotension (86/56), bloody oral mucous membranes, with normal heart rate and regular rhythm. Hemoglobin and platelets were 10.8gm/dL and 56k/µL, respectively. Subsequent esophagogastroduodenoscopy revealed a large quantity of food, blood clots in fundus and duodenum, and a normal esophagus. Since no other site of gastrointestinal bleeding on CT angiogram and splenorenal portosystemic collaterals were identified, a presumptive diagnosis of gastric varices was made. PaRTO was performed. Within an hour of PaRTO, the patient had chills, temperature of 103.2°F, tachycardia (120 bpm), transient hypertension (126/55) followed by hypotension (102/43), and had three bloody stools. Hypotension was refractory to administration of vasopressors (5 mcg/min of Levophed increased to 22 mcg/min), IV fluid bolus, and PRBCs. However, after 100mg IV hydrocortisone (Solu-Cortef) was given, blood pressure stabilized to 122/70 the next day.
Discussion: Gastrointestinal bleeding and cirrhosis are problems commonly encountered by gastroenterologists. Timely fluid resuscitation and investigation of the underlying cause of the patient's hypotension led to the prompt diagnosis of primary adrenal insufficiency (PAI) status post PARTO. A possible explanation for our patient’s complication was a transient occlusion of the adrenal vein during PaRTO since the patient had gastrorenal shunts. Suspecting transient adrenal insufficiency as a post-PaRTO complication can lead to better outcomes for treatment. More research needs to be done to investigate which patients are at a higher risk for adrenal insufficiency status post PaRTO.
Disclosures:
Eduardo A. Canto, BS1, Suhail Sidhu, BS1, Evan Daugherty, MD2, Nikhil Jagan, MBBS2, Avanija Kanmanthareddy, MBBS2, Rajani Rangray, MBBS2. P1093 - A Case of Adrenal Insufficiency Post PaRTO Procedure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: 630,000 adults in the United States live with cirrhosis. Variceal rupture is the deadliest complication from cirrhosis with a 20% mortality within six weeks after onset of hemorrhage. To manage portal hypertension secondary to chronic liver disease and prevent gastric varix rupture, plug-assisted retrograde transvenous obliteration (PaRTO) may be performed. Our case is the second of its kind to demonstrate transient adrenal insufficiency, a rare but life threatening complication, status post PaRTO.
Case Description/Methods: A 42 year-old man with past medical history of alcoholic liver cirrhosis with type I isolated gastric varices and a bleeding esophageal ulcer that required hemostatic spray presented with complaints of epigastric pain after an episode of hematemesis associated with lightheadedness and dizziness. Physical exam revealed scleral icterus, jaundice, RUQ abdominal tenderness, hypotension (86/56), bloody oral mucous membranes, with normal heart rate and regular rhythm. Hemoglobin and platelets were 10.8gm/dL and 56k/µL, respectively. Subsequent esophagogastroduodenoscopy revealed a large quantity of food, blood clots in fundus and duodenum, and a normal esophagus. Since no other site of gastrointestinal bleeding on CT angiogram and splenorenal portosystemic collaterals were identified, a presumptive diagnosis of gastric varices was made. PaRTO was performed. Within an hour of PaRTO, the patient had chills, temperature of 103.2°F, tachycardia (120 bpm), transient hypertension (126/55) followed by hypotension (102/43), and had three bloody stools. Hypotension was refractory to administration of vasopressors (5 mcg/min of Levophed increased to 22 mcg/min), IV fluid bolus, and PRBCs. However, after 100mg IV hydrocortisone (Solu-Cortef) was given, blood pressure stabilized to 122/70 the next day.
Discussion: Gastrointestinal bleeding and cirrhosis are problems commonly encountered by gastroenterologists. Timely fluid resuscitation and investigation of the underlying cause of the patient's hypotension led to the prompt diagnosis of primary adrenal insufficiency (PAI) status post PARTO. A possible explanation for our patient’s complication was a transient occlusion of the adrenal vein during PaRTO since the patient had gastrorenal shunts. Suspecting transient adrenal insufficiency as a post-PaRTO complication can lead to better outcomes for treatment. More research needs to be done to investigate which patients are at a higher risk for adrenal insufficiency status post PaRTO.
Disclosures:
Eduardo Canto indicated no relevant financial relationships.
Suhail Sidhu indicated no relevant financial relationships.
Evan Daugherty indicated no relevant financial relationships.
Nikhil Jagan indicated no relevant financial relationships.
Avanija Kanmanthareddy indicated no relevant financial relationships.
Rajani Rangray indicated no relevant financial relationships.
Eduardo A. Canto, BS1, Suhail Sidhu, BS1, Evan Daugherty, MD2, Nikhil Jagan, MBBS2, Avanija Kanmanthareddy, MBBS2, Rajani Rangray, MBBS2. P1093 - A Case of Adrenal Insufficiency Post PaRTO Procedure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
