Sunday Poster Session
Category: Liver
P1140 - Ascites in a Lupus Patient: A Diagnostic Conundrum
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Ixel Cervera, MD
NYU Langone Hospital-Brooklyn
New York, NY
Presenting Author(s)
Ixel Cervera, MD1, Navina Mohan, MD1, Jonathan Fricchione, MD1, Julia Cherkasova, DO1, Saikiran Kilaru, MD2
1NYU Langone Hospital-Brooklyn, Brooklyn, NY; 2NYU Langone Health, New York, NY
Introduction: Etiology of abdominal ascites in individuals with systemic lupus erythematosus varies greatly. A high index of suspicion, thorough cardiovascular, renal, hepatic, infectious, and malignant workup is required to identify the cause and elect treatment.
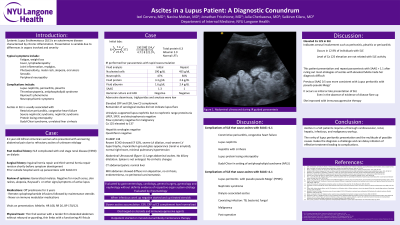
Case Description/Methods: A 41yo woman with a 20yr history of SLE complicated by ESRD for 7yrs presented with severe abdominal pain and distention. She stopped going to dialysis a month prior due to malaise. She was afebrile HR108 RR26 BP170/121. Exam showed a distended firm tender abdomen, no pedal edema. Labs revealed Hgb7.4 Hct22.6 WBC8.4 Plt 371 BUN 124 Cr 21.5, serum albumin 2.9 troponin 0.148 ESR30 CRP14.8 BNP 138 procalcitonin 1.13. CA125 prior month was 137. SPEP/UPEP, flow cytometry, and infectious serologies were negative. Unremarkable EKG. Abdominal US showed large ascites, echogenic atrophic kidneys, no cirrhosis, and non-enlarged spleen with calcified granulomas. Hepatic and portal veins were patent. CXR had no pleural effusion. TTE showed a 62% EF, left atrial and ventricular dilation, myocardium with ground-glass appearance. MRI abdomen revealed diffuse hepatic iron distribution, no cirrhosis or focal liver lesions, and no peritoneal carcinomatosis, a 2.4cm left ovarian endometrioma and a 2.2cm right paraovarian simple cyst. She received 2hrs of emergent HD, and large volume paracentesis. Peritoneal fluid showed a SAAG of 1.3, fluid protein 3.3g/dL, 190 nucleated cells, 24 RBCs. Negative fluid culture, AFB stain, and cytology. Steroids were started. Inflammatory markers normalized. Hydroxychloroquine and mycophenolate were added. Repeat LVP showed a SAAG of 1. Initiation of immunosuppression significantly slowed ascites accumulation and extended the time required between therapeutic LVP.
Discussion: Ascites is peritoneal fluid accumulation from hepatic, renal, or cardiac etiologies. Common causes include congestive heart failure, nephrotic syndrome, and decompensated cirrhosis. Less common ones include protein-losing enteropathy, Budd-Chiari syndrome, restrictive pericarditis, and peritoneal serositis related to SLE. It is important to not anchor on volume overload. This patient’s ascites was likely related to peritoneal serositis as evidenced by her ascites studies and improvement with SLE treatment. It is an unusual presentation of pseudo-pseudo Meigs' syndrome, defined by ascites, pleural effusions, and elevated CA125 level in patients with SLE. To make this diagnosis, gynecologic malignancy and Meigs' syndrome must be ruled out.

Disclosures:
Ixel Cervera, MD1, Navina Mohan, MD1, Jonathan Fricchione, MD1, Julia Cherkasova, DO1, Saikiran Kilaru, MD2. P1140 - Ascites in a Lupus Patient: A Diagnostic Conundrum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1NYU Langone Hospital-Brooklyn, Brooklyn, NY; 2NYU Langone Health, New York, NY
Introduction: Etiology of abdominal ascites in individuals with systemic lupus erythematosus varies greatly. A high index of suspicion, thorough cardiovascular, renal, hepatic, infectious, and malignant workup is required to identify the cause and elect treatment.
Case Description/Methods: A 41yo woman with a 20yr history of SLE complicated by ESRD for 7yrs presented with severe abdominal pain and distention. She stopped going to dialysis a month prior due to malaise. She was afebrile HR108 RR26 BP170/121. Exam showed a distended firm tender abdomen, no pedal edema. Labs revealed Hgb7.4 Hct22.6 WBC8.4 Plt 371 BUN 124 Cr 21.5, serum albumin 2.9 troponin 0.148 ESR30 CRP14.8 BNP 138 procalcitonin 1.13. CA125 prior month was 137. SPEP/UPEP, flow cytometry, and infectious serologies were negative. Unremarkable EKG. Abdominal US showed large ascites, echogenic atrophic kidneys, no cirrhosis, and non-enlarged spleen with calcified granulomas. Hepatic and portal veins were patent. CXR had no pleural effusion. TTE showed a 62% EF, left atrial and ventricular dilation, myocardium with ground-glass appearance. MRI abdomen revealed diffuse hepatic iron distribution, no cirrhosis or focal liver lesions, and no peritoneal carcinomatosis, a 2.4cm left ovarian endometrioma and a 2.2cm right paraovarian simple cyst. She received 2hrs of emergent HD, and large volume paracentesis. Peritoneal fluid showed a SAAG of 1.3, fluid protein 3.3g/dL, 190 nucleated cells, 24 RBCs. Negative fluid culture, AFB stain, and cytology. Steroids were started. Inflammatory markers normalized. Hydroxychloroquine and mycophenolate were added. Repeat LVP showed a SAAG of 1. Initiation of immunosuppression significantly slowed ascites accumulation and extended the time required between therapeutic LVP.
Discussion: Ascites is peritoneal fluid accumulation from hepatic, renal, or cardiac etiologies. Common causes include congestive heart failure, nephrotic syndrome, and decompensated cirrhosis. Less common ones include protein-losing enteropathy, Budd-Chiari syndrome, restrictive pericarditis, and peritoneal serositis related to SLE. It is important to not anchor on volume overload. This patient’s ascites was likely related to peritoneal serositis as evidenced by her ascites studies and improvement with SLE treatment. It is an unusual presentation of pseudo-pseudo Meigs' syndrome, defined by ascites, pleural effusions, and elevated CA125 level in patients with SLE. To make this diagnosis, gynecologic malignancy and Meigs' syndrome must be ruled out.

Figure: IR guided paracentesis drain placement
Disclosures:
Ixel Cervera indicated no relevant financial relationships.
Navina Mohan indicated no relevant financial relationships.
Jonathan Fricchione indicated no relevant financial relationships.
Julia Cherkasova indicated no relevant financial relationships.
Saikiran Kilaru indicated no relevant financial relationships.
Ixel Cervera, MD1, Navina Mohan, MD1, Jonathan Fricchione, MD1, Julia Cherkasova, DO1, Saikiran Kilaru, MD2. P1140 - Ascites in a Lupus Patient: A Diagnostic Conundrum, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
