Sunday Poster Session
Category: Liver
P1144 - Hepatocellular Carcinoma in the Setting of Autoimmune Hepatitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Smriti Kochhar, DO
Penn State Health Milton S. Hershey Medical Center
Edison, NJ
Presenting Author(s)
Smriti Kochhar, DO1, Monica Dzwonkowski, DO2, Deepa Kumarjiguda, DO2, Sanjeev Shrestha, MD2
1Penn State Health Milton S. Hershey Medical Center, Edison, NJ; 2Geisinger Medical Center, Danville, PA
Introduction: Autoimmune hepatitis (AIH) is an inflammatory liver condition characterized by circulating autoantibodies. Within a 10-year period, approximately 40% of AIH patients develop histologic cirrhosis, but their disease typically remains stable without decompensation or shortened survival. The incidence of hepatocellular carcinoma (HCC) in AIH patients is rare, around 1.007% per year. Due to this rarity, there are currently no screening guidelines for HCC screening in AIH patients. Here, we present a case of a patient with known AIH who was diagnosed with HCC despite having previously compensated cirrhosis, in the context of a recent pulmonary embolism (PE).
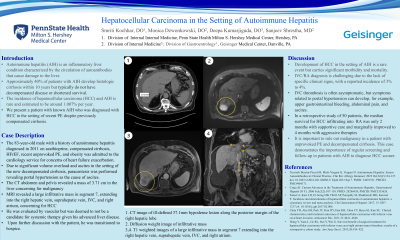
Case Description/Methods: An 83-year-old male was admitted to the cardiology service for concerns of heart failure exacerbation resistant to outpatient diuretic treatment. He presented with dyspnea on exertion and 10lb weight gain in the setting of dietary indiscretion. His past medical history was significant for autoimmune hepatitis diagnosed in 2011 for which he was on azathioprine, compensated cirrhosis, coronary artery disease with several coronary stents, heart failure with preserved ejection fraction, and recent unprovoked PE. He was treated with several days of intravenous diuretics with minimal improvement of swelling and urine output. Due to significant volume overload and ascites in the setting of decompensated cirrhosis, paracentesis was performed. Fluid analysis from paracentesis revealed portal hypertension as the cause of ascites and no concern for infection. A computed tomography scan of the abdomen and pelvis revealed a mass in the liver concerning for malignancy. Further workup with magnetic resonance imaging revealed a large infiltrative mass in segment 7, extending into the right hepatic vein, suprahepatic IVC and right atrium, concerning for HCC. Last screening abdominal ultrasound was over a year prior to presentation. He was evaluated by vascular surgery who did not think he was a candidate for invasive therapies for his clot, and he was deemed to not be a candidate for systemic therapy given his advanced liver disease. Upon further discussion with the patient, he was transitioned to hospice.
Discussion: Development of HCC in the setting of AIH is a rare event but carries significant morbidity and mortality. It is important to rule out malignancy in a patient with unprovoked PE and decompensated cirrhosis. This case demonstrates the importance of regular screening and follow-up in patients with AIH to diagnose HCC sooner.
Disclosures:
Smriti Kochhar, DO1, Monica Dzwonkowski, DO2, Deepa Kumarjiguda, DO2, Sanjeev Shrestha, MD2. P1144 - Hepatocellular Carcinoma in the Setting of Autoimmune Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Edison, NJ; 2Geisinger Medical Center, Danville, PA
Introduction: Autoimmune hepatitis (AIH) is an inflammatory liver condition characterized by circulating autoantibodies. Within a 10-year period, approximately 40% of AIH patients develop histologic cirrhosis, but their disease typically remains stable without decompensation or shortened survival. The incidence of hepatocellular carcinoma (HCC) in AIH patients is rare, around 1.007% per year. Due to this rarity, there are currently no screening guidelines for HCC screening in AIH patients. Here, we present a case of a patient with known AIH who was diagnosed with HCC despite having previously compensated cirrhosis, in the context of a recent pulmonary embolism (PE).
Case Description/Methods: An 83-year-old male was admitted to the cardiology service for concerns of heart failure exacerbation resistant to outpatient diuretic treatment. He presented with dyspnea on exertion and 10lb weight gain in the setting of dietary indiscretion. His past medical history was significant for autoimmune hepatitis diagnosed in 2011 for which he was on azathioprine, compensated cirrhosis, coronary artery disease with several coronary stents, heart failure with preserved ejection fraction, and recent unprovoked PE. He was treated with several days of intravenous diuretics with minimal improvement of swelling and urine output. Due to significant volume overload and ascites in the setting of decompensated cirrhosis, paracentesis was performed. Fluid analysis from paracentesis revealed portal hypertension as the cause of ascites and no concern for infection. A computed tomography scan of the abdomen and pelvis revealed a mass in the liver concerning for malignancy. Further workup with magnetic resonance imaging revealed a large infiltrative mass in segment 7, extending into the right hepatic vein, suprahepatic IVC and right atrium, concerning for HCC. Last screening abdominal ultrasound was over a year prior to presentation. He was evaluated by vascular surgery who did not think he was a candidate for invasive therapies for his clot, and he was deemed to not be a candidate for systemic therapy given his advanced liver disease. Upon further discussion with the patient, he was transitioned to hospice.
Discussion: Development of HCC in the setting of AIH is a rare event but carries significant morbidity and mortality. It is important to rule out malignancy in a patient with unprovoked PE and decompensated cirrhosis. This case demonstrates the importance of regular screening and follow-up in patients with AIH to diagnose HCC sooner.
Disclosures:
Smriti Kochhar indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Deepa Kumarjiguda indicated no relevant financial relationships.
Sanjeev Shrestha indicated no relevant financial relationships.
Smriti Kochhar, DO1, Monica Dzwonkowski, DO2, Deepa Kumarjiguda, DO2, Sanjeev Shrestha, MD2. P1144 - Hepatocellular Carcinoma in the Setting of Autoimmune Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
