Sunday Poster Session
Category: Obesity
P1171 - Delayed Vertical Banded Gastroplasty Complication and Resolution by Gastric Band Transection
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Jonathan Ragheb, MD
Cleveland Clinic Florida
Weston, FL
Presenting Author(s)
Alec Swartz, BS1, Jonathan Ragheb, MD2, Mohammad Alomari, MD2, Frances Tardy Rivera, MD2, Ashraf Almomani, MD2, Pravallika Chadalavada, MD2, Hammad Zafar, MD2, Mamoon Ur Rashid, MD3, Ronnie Pimentel, MD, FACG2
1Ross University School of Medicine, Weston, FL; 2Cleveland Clinic Florida, Weston, FL; 3Cleveland Clinic, Weston, FL
Introduction: Vertical banded gastroplasty (VBG) is a restrictive weight loss procedure commonly performed in the 1980s-early 2000s. Most complications present within the first 4 years postoperatively, necessitating revision in approximately 50% of patients. This case examines an atypical instance of delayed staple line leak revised laparoscopically.
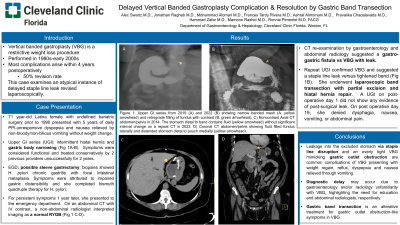
Case Description/Methods: A 71 year-old Hispanic female with a history of bariatric surgery more than 30 years prior presented with 5 years of daily postprandial epigastric pain, bloating, and nausea relieved by non-bloody/non-bilious vomiting without weight change since symptom onset. Symptoms did not improve with PPI. An upper GI series (UGI) revealed a small intermittent hiatal hernia and narrowing of the gastric body, consistent with previous gastric surgery (Fig 1A). Given chronicity, symptoms were considered functional and treated conservatively by 2 previous providers without resolution. Two years later she underwent an esophagogastroduodenoscopy; gastric biopsies showed chronic gastritis with focal intestinal metaplasia and active H. pylori. Endoscopically, there were no signs of Roux-en-y gastric bypass (RYGB), and providers considered these findings consistent with sleeve gastrectomy, attributing symptoms to impaired gastric distensibility. She was given bismuth quadruple therapy for H. pylori and continued on PPIs. One year later she presented to the emergency department with persistent symptoms. On an abdominal CT with IV contrast a non-abdominal radiologist interpreted imaging as a normal RYGB (Fig 1 C-D). Gastroenterology was consulted, and re-examination of the CT suggested a gastro-gastric fistula versus VBG with leak based on a fluid collection identified in the excluded stomach. An UGI series confirmed VBG and suggested a staple line leak versus tightened band (Fig 1B). She underwent laparoscopic band transection with partial excision and hiatal hernia repair by general surgery. An upper GI series on post-operative day 1 did not show any evidence of post-surgical leak. On follow up post operative day 19, she had no dysphagia, nausea, vomiting, or abdominal pain.
Discussion: We present a delayed diagnosis of tight VBG which demonstrates the need for physician awareness of early bariatric procedures. This case also highlights the importance of including abdominal radiologists in management of patients requesting second opinions. Lastly, gastric band transection can be considered as an alternative to other VBG revision approaches, such as RYGB.

Disclosures:
Alec Swartz, BS1, Jonathan Ragheb, MD2, Mohammad Alomari, MD2, Frances Tardy Rivera, MD2, Ashraf Almomani, MD2, Pravallika Chadalavada, MD2, Hammad Zafar, MD2, Mamoon Ur Rashid, MD3, Ronnie Pimentel, MD, FACG2. P1171 - Delayed Vertical Banded Gastroplasty Complication and Resolution by Gastric Band Transection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Ross University School of Medicine, Weston, FL; 2Cleveland Clinic Florida, Weston, FL; 3Cleveland Clinic, Weston, FL
Introduction: Vertical banded gastroplasty (VBG) is a restrictive weight loss procedure commonly performed in the 1980s-early 2000s. Most complications present within the first 4 years postoperatively, necessitating revision in approximately 50% of patients. This case examines an atypical instance of delayed staple line leak revised laparoscopically.
Case Description/Methods: A 71 year-old Hispanic female with a history of bariatric surgery more than 30 years prior presented with 5 years of daily postprandial epigastric pain, bloating, and nausea relieved by non-bloody/non-bilious vomiting without weight change since symptom onset. Symptoms did not improve with PPI. An upper GI series (UGI) revealed a small intermittent hiatal hernia and narrowing of the gastric body, consistent with previous gastric surgery (Fig 1A). Given chronicity, symptoms were considered functional and treated conservatively by 2 previous providers without resolution. Two years later she underwent an esophagogastroduodenoscopy; gastric biopsies showed chronic gastritis with focal intestinal metaplasia and active H. pylori. Endoscopically, there were no signs of Roux-en-y gastric bypass (RYGB), and providers considered these findings consistent with sleeve gastrectomy, attributing symptoms to impaired gastric distensibility. She was given bismuth quadruple therapy for H. pylori and continued on PPIs. One year later she presented to the emergency department with persistent symptoms. On an abdominal CT with IV contrast a non-abdominal radiologist interpreted imaging as a normal RYGB (Fig 1 C-D). Gastroenterology was consulted, and re-examination of the CT suggested a gastro-gastric fistula versus VBG with leak based on a fluid collection identified in the excluded stomach. An UGI series confirmed VBG and suggested a staple line leak versus tightened band (Fig 1B). She underwent laparoscopic band transection with partial excision and hiatal hernia repair by general surgery. An upper GI series on post-operative day 1 did not show any evidence of post-surgical leak. On follow up post operative day 19, she had no dysphagia, nausea, vomiting, or abdominal pain.
Discussion: We present a delayed diagnosis of tight VBG which demonstrates the need for physician awareness of early bariatric procedures. This case also highlights the importance of including abdominal radiologists in management of patients requesting second opinions. Lastly, gastric band transection can be considered as an alternative to other VBG revision approaches, such as RYGB.

Figure: Figure 1. Upper GI series from 2019 (A) and 2022 (B) showing narrow banded mesh (A; yellow arrowhead) and retrograde filling of fundus with contrast (B; green arrowhead). Coronal CT abdomen and pelvis without IV contrast showing fluid filled fundus laterally and distended stomach distal to pouch medially (C-D, arrowhead).
Disclosures:
Alec Swartz indicated no relevant financial relationships.
Jonathan Ragheb: Abbvie – Food/Beverage. Janssen Pharmaceuticals, Inc – Education, Food/Beverage. Medtronic – Food/Beverage. Takeda Pharmaceuticals – Food/Beverage.
Mohammad Alomari indicated no relevant financial relationships.
Frances Tardy Rivera: Siemens Medical Solutions – Food & Beverage.
Ashraf Almomani indicated no relevant financial relationships.
Pravallika Chadalavada indicated no relevant financial relationships.
Hammad Zafar indicated no relevant financial relationships.
Mamoon Ur Rashid indicated no relevant financial relationships.
Ronnie Pimentel: Boston Scientific – Food & Beverage.
Alec Swartz, BS1, Jonathan Ragheb, MD2, Mohammad Alomari, MD2, Frances Tardy Rivera, MD2, Ashraf Almomani, MD2, Pravallika Chadalavada, MD2, Hammad Zafar, MD2, Mamoon Ur Rashid, MD3, Ronnie Pimentel, MD, FACG2. P1171 - Delayed Vertical Banded Gastroplasty Complication and Resolution by Gastric Band Transection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
