Sunday Poster Session
Category: Practice Management
P1208 - Reflections of a Newly Implemented Percutaneous Endoscopic Gastrostomy Tube Workflow
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Emily S. Seltzer, DO, MS
Mount Sinai West and Morningside
New York, New York
Presenting Author(s)
Emily S. Seltzer, DO, MS1, Erica Park, MD2, Patricia Miguez Arosemena, MD1, Ines Varela, MD3, Anudeep Neelam, MD4, Michael S.. Smith, MD, MBA5, Priya Simoes, MD2
1Mount Sinai West and Morningside, New York, NY; 2Mount Sinai Morningside and West, New York, NY; 3Mount Sinai West/Morningside Hospitals, New York, NY; 4Mount Sinai Morningside West, New York, NY; 5Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The decision for Percutaneous Endoscopic Gastrostomy (PEG) tube placement involves a comprehensive assessment, considering patient-centered factors and contraindications. Guidelines recommend pre-procedure checklists to enhance patient safety. This study describes the experience of primary providers and gastroenterology (GI) consultants' use of a novel checklist-based workflow for PEG tube placement.
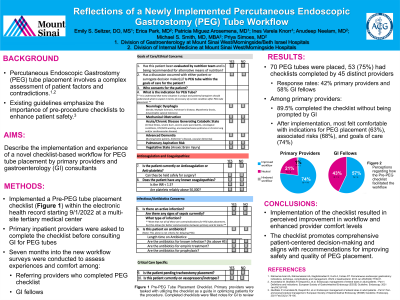
Methods: A Pre-PEG tube checklist (Figure 1) was implemented from 9/1/22 to 4/17/23 within the electronic health record of a multi-site tertiary medical center. Primary inpatient providers were asked to complete the checklist before consulting GI for PEGs. Surveys were conducted among referring providers and GI fellows regarding their experiences and comfort level surrounding PEG tube consultations.
Results: Out of 70 PEG placements during the study period, 53 had the checklist completed by 45 distinct providers. The completion rates for primary provider and GI fellow surveys were 42% and 58%, respectively. Among residents and advanced practice providers (APPs), 74% felt the intervention improved workflow. Among GI fellows, 100% believed it improved workflow or felt neutral, with none perceiving it as a hindrance. Most providers (89.5%) completed the checklist unprompted before consulting GI. After completing the checklist, the majority of residents and APPs felt comfortable with indications for PEG placement (63%), associated risks (68%), and goals of care discussions (74%). However, 37% felt influenced by primary service attendings to consult GI despite patients not meeting optimization parameters. Primary providers and fellows identified goals of care discussions, disposition planning barriers, and scheduling issues as common reasons for delays in PEG placement.
Discussion: Implementation of the pre-PEG tube checklist improved workflow and enhanced provider comfort levels. The high completion rate and positive provider feedback demonstrate effectiveness in streamlining the GI consultative process. The checklist promotes comprehensive patient-centered decision-making and aligns with recommendations for improving the safety and quality of PEG placement. Future interventions will build upon these findings to optimize the checklist and promote even more efficient and patient-centered care.

Disclosures:
Emily S. Seltzer, DO, MS1, Erica Park, MD2, Patricia Miguez Arosemena, MD1, Ines Varela, MD3, Anudeep Neelam, MD4, Michael S.. Smith, MD, MBA5, Priya Simoes, MD2. P1208 - Reflections of a Newly Implemented Percutaneous Endoscopic Gastrostomy Tube Workflow, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai West and Morningside, New York, NY; 2Mount Sinai Morningside and West, New York, NY; 3Mount Sinai West/Morningside Hospitals, New York, NY; 4Mount Sinai Morningside West, New York, NY; 5Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The decision for Percutaneous Endoscopic Gastrostomy (PEG) tube placement involves a comprehensive assessment, considering patient-centered factors and contraindications. Guidelines recommend pre-procedure checklists to enhance patient safety. This study describes the experience of primary providers and gastroenterology (GI) consultants' use of a novel checklist-based workflow for PEG tube placement.
Methods: A Pre-PEG tube checklist (Figure 1) was implemented from 9/1/22 to 4/17/23 within the electronic health record of a multi-site tertiary medical center. Primary inpatient providers were asked to complete the checklist before consulting GI for PEGs. Surveys were conducted among referring providers and GI fellows regarding their experiences and comfort level surrounding PEG tube consultations.
Results: Out of 70 PEG placements during the study period, 53 had the checklist completed by 45 distinct providers. The completion rates for primary provider and GI fellow surveys were 42% and 58%, respectively. Among residents and advanced practice providers (APPs), 74% felt the intervention improved workflow. Among GI fellows, 100% believed it improved workflow or felt neutral, with none perceiving it as a hindrance. Most providers (89.5%) completed the checklist unprompted before consulting GI. After completing the checklist, the majority of residents and APPs felt comfortable with indications for PEG placement (63%), associated risks (68%), and goals of care discussions (74%). However, 37% felt influenced by primary service attendings to consult GI despite patients not meeting optimization parameters. Primary providers and fellows identified goals of care discussions, disposition planning barriers, and scheduling issues as common reasons for delays in PEG placement.
Discussion: Implementation of the pre-PEG tube checklist improved workflow and enhanced provider comfort levels. The high completion rate and positive provider feedback demonstrate effectiveness in streamlining the GI consultative process. The checklist promotes comprehensive patient-centered decision-making and aligns with recommendations for improving the safety and quality of PEG placement. Future interventions will build upon these findings to optimize the checklist and promote even more efficient and patient-centered care.

Figure: Figure 1. Pre-Percutaneous Endoscopic Gastrostomy (PEG) Tube Placement Consult Checklist. Primary team providers are expected to use the checklist as a guide to ensure patient optimization prior to consulting gastroenterology. Teams are asked complete this checklist within the electronic medical record.
Disclosures:
Emily Seltzer indicated no relevant financial relationships.
Erica Park indicated no relevant financial relationships.
Patricia Miguez Arosemena indicated no relevant financial relationships.
Ines Varela indicated no relevant financial relationships.
Anudeep Neelam indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Medical – Consultant. Steris Endoscopy – Consultant.
Priya Simoes indicated no relevant financial relationships.
Emily S. Seltzer, DO, MS1, Erica Park, MD2, Patricia Miguez Arosemena, MD1, Ines Varela, MD3, Anudeep Neelam, MD4, Michael S.. Smith, MD, MBA5, Priya Simoes, MD2. P1208 - Reflections of a Newly Implemented Percutaneous Endoscopic Gastrostomy Tube Workflow, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

